🔗Preface
 |  |
Before and after
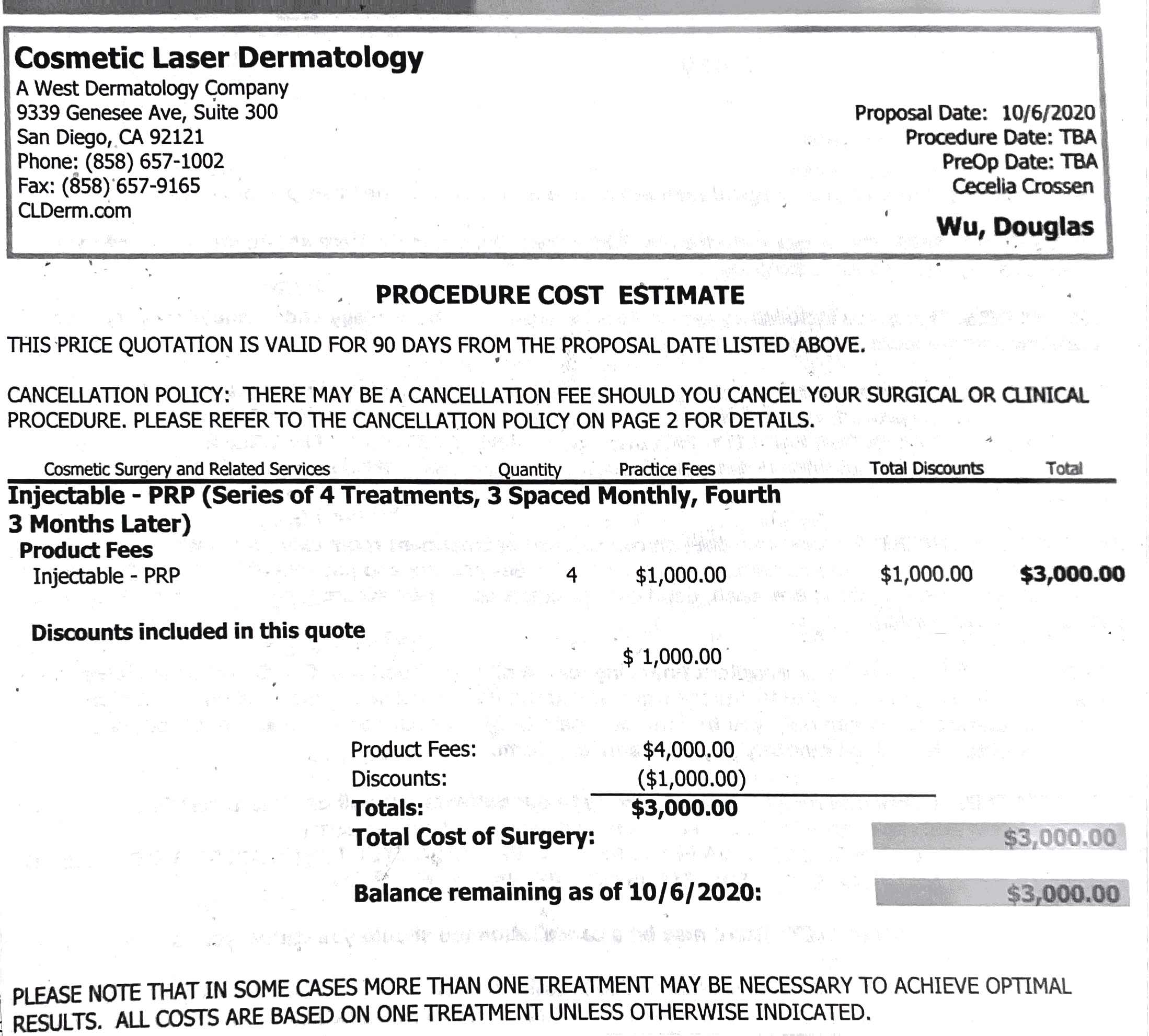
Below is a chronological account of my biggest regret in life, trusting Dr. Douglas Wu to perform a CO2 laser on me. It is accompanied by medical records, photos, and references to research articles. I am so sorry to any of Dr. Wu’s patients who could have used this info for how long after this incident I’ve waited to share my story. It took me a long time to figure out what was going on; to find other, competent doctors who could help; to understand what channels I could seek accountability through and let those processes play out; and just to power through the intense emotions that would come up every time I tried to write and was overwhelemed by the trauma I’ve endured. Some things to keep in mind as you read through this are that I went into this not knowing anything about this procedure since it was Dr. Wu who suggested and introduced it to me, never having had a surgery before (yes, both CO2 laser and subcision are classified as surgery according to the AMA, which was never made clear to me), never having had a laser before, and with a naïve trust that Dr. Wu had my best interest at heart since he “feels like his [20,000+] patients are like family”↗. I acknowledge that I ignored red flags because of my insecurity about my acne scarring that I was desperate to address (my perception of the severity of which was clouded and amplified by then-undiagnosed psychological issues like body dysmorphia) and Dr. Wu’s confidence, and that I did not ask enough questions because I thought Dr. Wu would appropriately inform me of any risks and how to identify and prevent them.
🔗Table of Contents
- Intro
- 1. Dr. Wu’s Treatment Prescriptions
- 2. Evaluating My Candidacy for CO2 Laser
- 3. Procedure Issues
- 3.1. Safety Protocol and Instructions for CO2 Laser on My Back
- 3.2. Pre-Op Concerns for CO2 Laser on My Face
- 3.3. Being Coerced to Sign the Consent Form Under Duress
- 3.4. Active Infection at the Procedure
- 3.5. Misinforming Me on the Intensity and Type of Procedure
- 3.6. Safety Protocols at the Procedure
- 3.7. Questionable Laser Settings
- 3.8. Post-op Instructions
- 4. Post-Procedure Issues
- 5. Getting Other Opinions
- 6. The Aftermath
- 7. Trouble Getting Medical Records
- 8. “Double Board Certification”
- 9. A Call for Restrictions on Who Can Perform Ablative CO2 Laser
- 10. Conclusion
- 11. Reporting the Incident
- References
🔗Intro
I saw Dr. Douglas C. Wu (CALIFORNIA PHYSICIAN AND SURGEON A License A 130151)↗ at his practice, Cosmetic Laser Dermatology, a West Dermatology company, in San Diego, California primarily for reconstructive treatment of atrophic acne scars between October 6, 2020, the date of our first consultation (in person), and March 8, 2022, the date I formally ended our doctor-patient relationship over email.
I found him because he and his practice appeared top rated on online review platforms and I had read an account online of him performing blunt-cannula subcision, the procedure I was specifically seeking out since neither of my two previous cosmetic-reconstruction doctors local to me performed it. His adjunct position as director of research at his apparently esteemed practice added to my confidence that he would be up to date on the most effective and safe treatments for the conditions he treats.
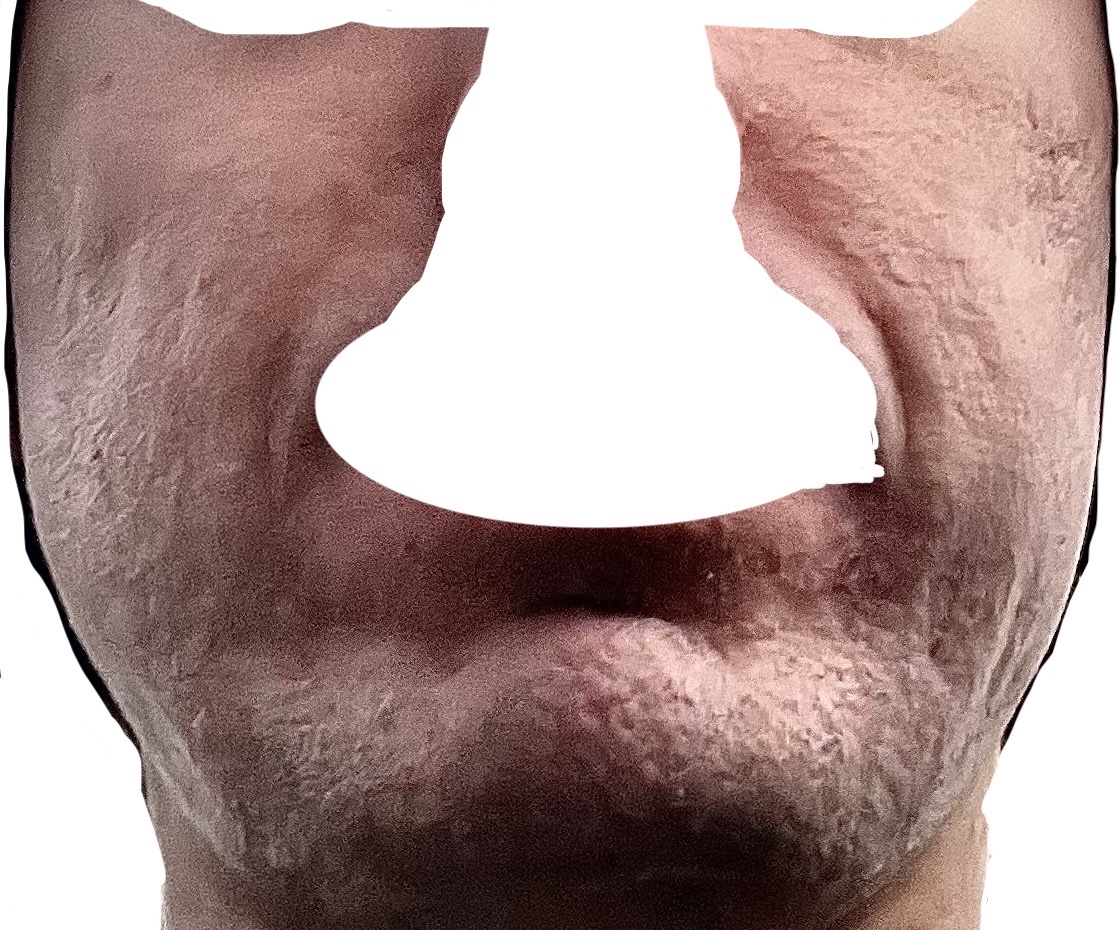
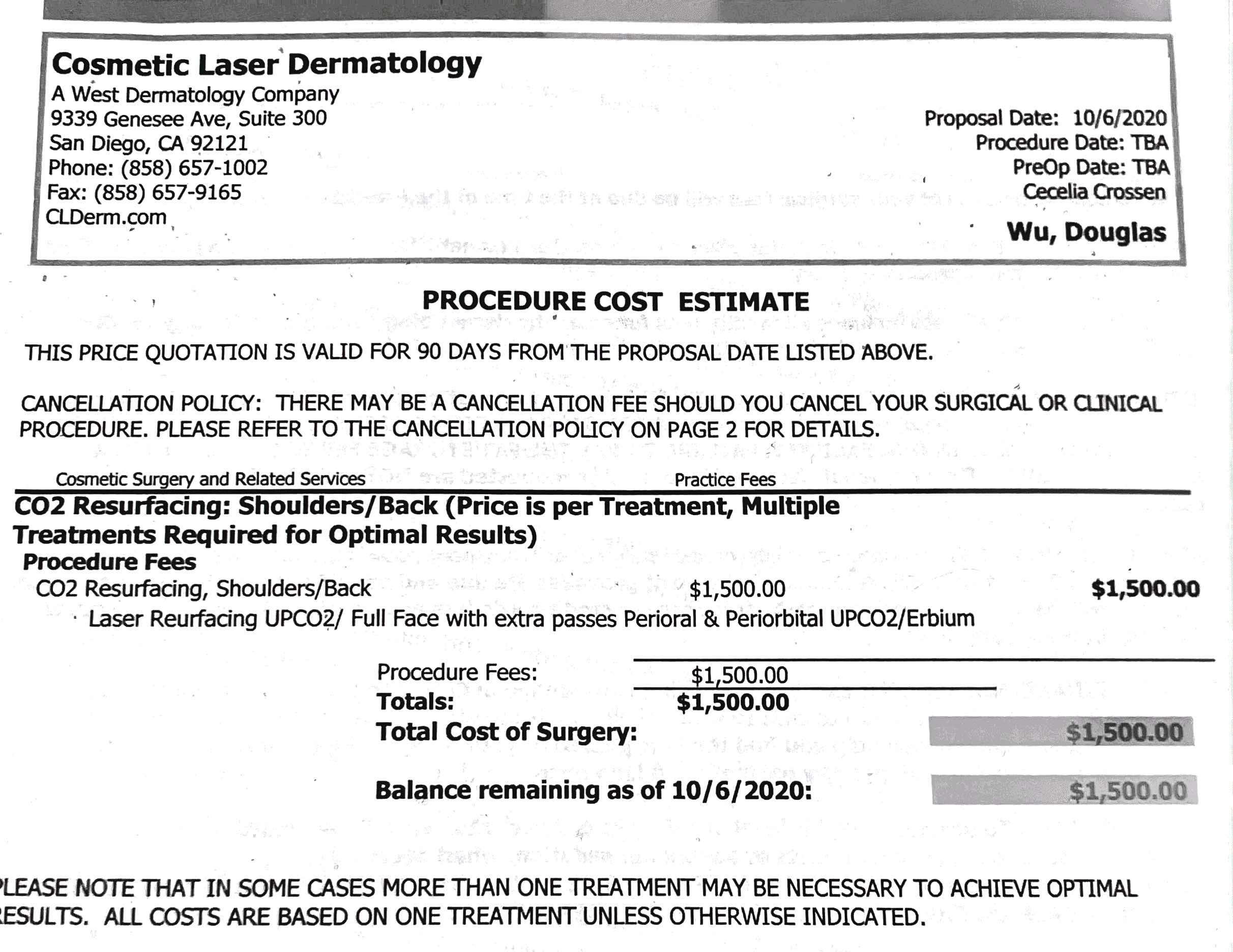
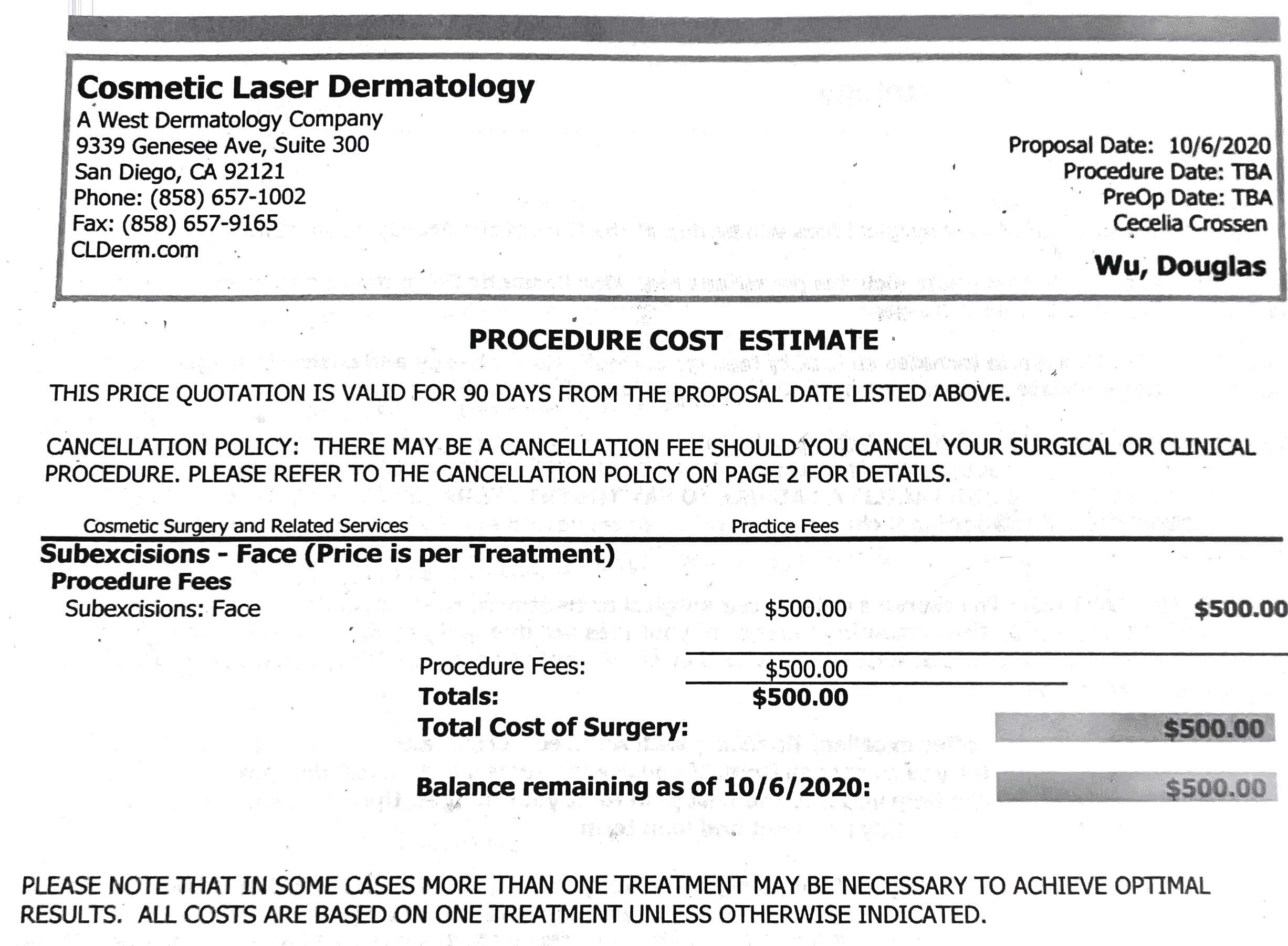
I followed all of Dr. Wu’s advice, putting together what the quotes he gave me (Figures 1-5) said and what he told me in consult and over email. He performed a subcision, a carbon dioxide (CO2) laser on my back, and a CO2 laser on my face (with another subcision—and subsequently other treatments he recommended after the fact, which I discuss in Section 4.6), as well as a course of 4 platelet-rich plasma (PRP) scalp injections for hair loss. I was, however, left with iatrogenic hypertrophic burn scarring over the entire treated area following the CO2 laser on my face.
🔗1. Dr. Wu’s Treatment Prescriptions
At the initial consultation, Dr. Wu confirmed I was a good candidate for subcision after tactilely confirming the distensibility of my atrophic scars on my cheeks and temples, the majority of which were classed as rolling. Dr. Wu informed me he preferred to use a combination of cannula and Nokor needles in the procedure, which I agreed to, trusting in his expertise. Dr. Wu also unsolicitedly recommended laser treatment. I asked instead about further radiofrequency (RF) microneedling, expressing that I hadn’t seen any positive results from 6 previous sessions that year constituting a treatment plan devised and executed by another doctor, and in fact it had left my face looking hollower, more textured, and with several hypertrophic scars. He told me I was not a candidate for further RF microneedling but that treating with a new modality, namely laser, would yield the most benefit in correcting the issues induced by RF microneedling as well as my acne scarring.
Dr. Wu said I could do fractional, non-ablative Fraxel® laser, but he seemed to dissuade me from that in saying I wouldn’t actually notice any perceptible improvement on my back and my face without doing fractionally ablative CO2 laser (fractionally ablative laser is also known as ablative fractional laser), which he called the “gold standard” for acne-scar treatment. This advice seems to conflict with Jalian et al.’s assessment in the study “Common Causes of Injury and Legal Action in Laser Surgery” that “Rejuvenation was the second most commonly litigated procedure. The vast majority of these procedures involved carbon dioxide resurfacing, a technique that has largely been abandoned because it involves a significant risk of hypopigmentation and scarring” (Jalian et al., 2013). Faghihi et al. also counter Dr. Wu’s authoritative claim in writing “There is no gold standard treatment for facial acne scars” (Faghihi et al., 2017), which paints Dr. Wu’s language as deceptive.
Dr. Wu lastly visually diagnosed me with male-pattern hair loss (androgenic/androgenetic alopecia). He did so without any of the standard tests such as hair count, pull test, trichogram, or trichoscopy (at least 10x magnification of the site looking for signs differentiating between various alopecias) (Jain et al., 2013). He prescribed PRP scalp injections, which he called the “gold standard” for hair-loss treatment in consult and again over email, another piece of advice that I later learned contradicts the leading advice in the field of male-pattern hair loss that finasteride and minoxidil are the gold standard (Tak et al., 2020).
Below are the complete documents Dr. Wu gave me for a “full-face” CO2 laser on the shoulders/back (Figure 1), a “full-face” CO2 laser on the face (Figure 2), “subexcisions” on the face (Figure 3), Fraxel® RE:Store Dual on the face (Figure 4), and PRP injections to the scalp (Figure 5). I believe “full face” refers to the full face of the affected area or scars in this case, since it appears on both quotes for the back and face. It is harder to interpret “with extra passes Perioral & Periorbital UPCO2/Erbium”, as it also appears on both quotes for the face and back. However, Dr. Wu never targeted those areas on my face (Figure 12), and those areas are exclusive to the face unless they are analogies to the mouth/eye of the scars. Lastly, I believe “subexcision” is meant to be subcision or subcutaneous incisionless surgery (Orentreich & Orentreich, 1995) rather than “excisional”, as Dr. Wu never made any mention of excising any tissue but rather severing the fibrous bands tethering the atrophic scars to underlying tissues via skin puncture.
Quote/procedure info for CO2 laser on my back

Quote/procedure info for CO2 laser on my face
Quote/procedure info for subcisions on my face

Quote/procedure info for Fraxel® laser on my face
Quote/procedure info for PRP injections on my scalp
🔗2. Evaluating My Candidacy for CO2 Laser
There are numerous factors I disclosed to Dr. Wu that I now believe made me a poor candidate for CO2 laser, or at least warranted added safety measures like testing, especially at the high settings he ended up using on my face. Other laser surgeons indicate some of these factors as absolute contraindications for CO2 laser.
🔗2.1. Hypertrophic Scar Tendency
I alerted Dr. Wu that I had formed several hypertrophic scars after RF microneedling procedures. He told me the CO2 laser was also the “gold standard” to treat these in consult and again over email (yes, he used that phrase that often), but many warn that history of forming hypertrophic scarring is a contraindication for the procedure in the first place (Horton & Alster, 1999) (Krupa Shankar et al., 2009) (Ramsdell, 2012). In light of this strong contraindication, I wish Dr. Wu would have informed me of the option to perform a test spot at the very least. These hypertrophic scars ultimately worsened (grew) after the CO2 laser he performed, and I later learned that there are other less invasive options with higher success rates like intralesional corticosteroid injection (Rabello et al., 2014) and electrodessication (e.g., Hyfrecator®) (P.R., M.D., in-person treatment, August 2, 2021-October 4, 2022.), among others, none of which Dr. Wu ever informed me of.
🔗2.2. Unsuitable Skin Type
I have learned since the procedure that I am a type 3 on the Fitzpatrick phototype scale↗. Dr. Wu did not ever determine my Fitzpatrick skin type, which could have been done by verbal assessment about if I burn and/or tan and my ethnic background or by reflectance spectroscopy (Sharma & Patel, 2022). This determination is especially important for CO2 laser as “carbon dioxide laser resurfacing produces its optimal results in patients with Fitzpatrick type I-II skin - fair-skinned Caucasians - because they have fewer melanocytes, which are prone to causing dyspigmentation as a result of post-procedure inflammation” (Yumeen & Khan, 2021). Yumeen and Khan proceed to elaborate, “Changes in pigmentation, both hyperpigmentation, and hypopigmentation, are also common. The risk of these changes is increased in Fitzpatrick skin types III-VI compared with types I-II” (Yumeen & Khan, 2021) (Metelitsa & Alster, 2010). I was not educated on the potential for these permanent changes, and I was not warned of their increased likelihood due to my skin type.
Furthermore, Dr. Wu did not give me any skin preparation protocol, which could have included “hydroquinone and glycolic acid in order to reduce the likelihood of dyspigmentation” (Sharma & Patel, 2022) (F., 2015). The operator manual for the UltraPulse device↗ (p148) reiterates this in instructing:
Subjects with an increased risk for hyperpigmentation, typically identified as having skin types III, IV, V and VI, should apply topical hydroquinones, such as Melanex®, or an equivalent depigmenting agent, twice daily, in the morning and evening, for a minimum of 2 weeks, preferably 4 to 6 weeks, prior to laser skin resurfacing.
Apfelberg indiscriminately advocates for a skin preparation protocol for UltraPulse CO2 laser patients, stating “Skin preparation with Retin-A and bleaching agents is important for best wound healing” (Apfelberg, 1997).
The UltraPulse manual↗ (p148) goes on to warn “Laser test patching should be considered prior to treatment, especially for subjects identified as having skin types III, IV, V and VI.” Once again, Dr. Wu never informed me of the option to do a test patch. The device instructions↗ elaborate on the significance of a test spot by listing as a contraindication patients who “demonstrate excessive or unusually prolonged erythema, hyperpigmentation, or hypopigmentation upon laser test patching” (p146). It does not seem Dr. Wu took my skin type into account in deciding what settings he would ultimately use either, as he only told me the morning after the CO2 laser procedure on my face that he used the strongest settings there are (Figure 12), whereas the nurses told me he was going to do a light treatment immediately before the procedure. One could surmise such strong settings are especially risky given the risk of this procedure at all in my skin type.
🔗2.3. Blood Disorder
I was diagnosed with a blood disease called heterozygous hemoglobin lepore on Sep 11, 2020 by endocrinologist Dr. A.P. He explained that it presents similarly to anemia on blood tests (high RBC count and RDW, and low MCV and MCH) and told me to inform doctors of it.
I indicated I have this disorder on the intake forms Dr. Wu’s staff had me fill out before our first consultation. Nevertheless, I expected that he may have missed it, so I made sure to ask him directly at the first consultation if this disorder was a contraindication for the CO2 laser he recommended. Dr. Wu said he wasn’t familiar with this disorder, and I incorrectly responded that I thought it affects white blood cells. Dr. Wu responded that white blood cells don’t matter with respect to these procedures and that I was still a good candidate. However, this advice alone seems to contradict the fact that “white blood cells help fight infection from germs and begin to repair the wound” (“How Wounds Heal,” n.d.).
I later realized this disorder, as the “hemoglobin” in its name implies, actually affects red blood cells and is related to sickle-cell disease and thalassemia. He did not look any further into it as far as I know, but Navratil and Kymplova say blood diseases could be a contraindication for laser or at least something that would warrant further probing or safety measures . This may be because hemoglobin abnormalities can predispose one to infection or prevent normal early wound healing (Mahajan et al., 2021). Ramsdell lists “diseases that inhibit healing” as a contraindication (Ramsdell, 2012a).
🔗2.4. Insufficient Time Since Previous Energy Treatments
After Dr. Wu recommended the CO2 laser at the initial consultation, I emailed Dr. Wu and his assistant, Cecelia Crossen, to remind him I had 6 RF microneedling treatments on my full face that year, the final one being less than a month before, and to ask if there was a certain amount of time I needed to wait to do further treatments, especially the CO2 laser, as I had just concluded the series of RF microneedling a month prior. Dr. Wu’s assistant, Cecelia, responded Oct 13, 2020 that Dr. Wu’s thoughts were “because Dr. Wu recommended a different modality to address your scarring, you do not need to wait 3-6 months because the treatment will not interfere with the collagen stimulation from that series. The only reason to wait is if you wish to see the full results from your series before beginning another treatment”. Dr. Wu did not ask for the procedure parameters from the RF microneedling, which several experts (P.R., M.D., in-person consultation, August 2, 2021. & J.P., M.D., in-person treatment, January 6, 2022.) later informed me were also extreme, before making that recommendation. Furthermore, Dr. Wu’s advice seems to contradict the advice that recent and/or excessive irradiation to or recent undermining of the skin to be treated is a contraindication for CO2 laser (Horton & Alster, 1999) (Verma et al., 2022). Lastly, many doctors I’ve seen since have directly countered Dr. Wu’s advice, explaining that damaging the skin, espcially with energy, too often will induce scarring.
🔗2.5. Unrealistic Expectations and No Mental Health Check
When Dr. Wu brought up temporary fillers in the initial consultation, I told him I was wary of them because of potential complications and lack of longevity. Dr. Wu said I was not a candidate for permanent ones like Bellafill® due to me being only 25 years old (this does not align with the advice of the manufacturer or other doctors). I believe unrealistic expectations were set, leading me to believe CO2 laser and Dr. Wu’s form of spot subcision would yield significant improvement in my atrophic scarring without diagnosing the source of volume loss; informing me of all alternatives; counseling me on all the potential complications and the potential for things to worsen so much, as they ultimately did; and assessing my mental ability to handle those consequences (Ramsdell, 2012a). Dr. Wu and his staff repeatedly advised me to do the CO2 laser specifically, praising it as a procedure I would only need one session of to yield substantial improvement in my particular case. He did not give me a full range of industry-standard treatment options (most with better safety profiles and some more effective than CO2 laser) like fat transfer (Azzam et al., 2013) (Zhang et al., 2022), Sculptra® (poly-L-lactic acid) (Sadick & Palmisano, 2009), full-field/extensive multilevel subcision (Taylor & Koron, 2021) (Rullan et al., 2020) (Taylor et al., 2017), chemical peels (Taylor & Koron, 2021) (Boen & Jacob, 2019), or erbium laser (Taylor & Koron, 2021) (Jeong et al., 2003)—or referral to experts who perform them.
Dr. Wu also neglected to investigate or regard my mental status at any point before or during treatment. Rabello et al. stress the mental and pathological importance of this step when undergoing scar treatment (Rabello et al., 2014):
It is important to investigate a patient’s current mental status to exclude the possibility of any psychiatric disorder before initiating treatment planning. Patients presenting a history of severe sadness or other depressive symptoms should be diagnosed and followed by a psychologist and psychiatrist and should start treatment only after discharge by the expert. Psychological stress also seems to be related to the recurrence of fibroproliferative scarring.
I had never seen a mental health specialist at that point, but I did experience significant anxiety due to my acne scarring, perhaps more than is typical, only heightened due to multiple previous procedures only seeming to worsen things. Aside from the factors that led to my misunderstanding of the procedures he prescribed (Section 3), a mental health evaluation might have determined I did not possess the mental faculties to understand the possible outcomes and limitations of his proposed treatments and therefore was not a good candidate.
🔗3. Procedure Issues
🔗3.1. Safety Protocol and Instructions for CO2 Laser on My Back
I first tried the CO2 laser on my back. As Dr. Wu never made me aware of the option to do a test spot, I figured starting with the part of my body that is usually covered was the safest way to see how I would respond. There was no pre-op appointment offered. I was not alerted to test for pulmonary tuberculosis given my diagnosis of latent tuberculosis I had previously disclosed. Neither was I asked to take a SARS-CoV-2 test. I now know both of these are relevant because any infections anywhere in the body cause abnormal healing. There was no antimicrobial prophylaxis offered, which I now know is standard for treatments of this intensity (Yumeen & Khan, 2021). There were no written instructions given to me nor verbal instructions other than to keep the area moist. Dr. Wu never informed me about risks like infection or permanent dyspigmentation. There was no follow-up given to me and nobody ever contacted me after the procedure to check up. No emergency contact info was given to me either. Dr. Wu never counseled me on the laser settings or device(s) he would use prior to treatment. He marked areas to be treated but did not show me or give me input on them. During the procedure, no eye protection was given. I was only instructed to close my eyes, which might seem reasonable since my back was being treated, but the ground I was facing laying down was reflective (Huang et al., 2018), as an aexample of the risk.
I therefore figured CO2 laser was a procedure no more risky than the microneedling, RF microneedling, or subcision I had previously had, not that Dr. Wu is negligent. I expressed concern several times in the following months over how long the redness was lasting, but Dr. Wu was confident in telling me that it was normal for the redness to linger for many months after and that it was indubitably a good thing because more inflammation meant more collagen was being produced for better results (never telling me that the type of collagen being formed is important since hypertrophic scars are an abundance of collagen). He told me this via email and virtual consult without even asking for photos of the area. Dr. Wu never made me aware that prolonged erythema can also indicate infection or delayed healing (Horton & Alster, 1999) (Ramsdell, 2012b) (Metelitsa & Alster, 2010). He never probed further. Nonetheless, I did not ultimately perceive significant adverse effects from this treatment other than laser gridding persisting to this day—nor did I see improvement, though Dr. Wu was confident in telling me “I’m definitely seeing some good improvements” and later “there seems to be noticeable improvement” over email with only his office’s over-exposed photos that didn’t show the issue well. When I responded with my own photo showing the issue, he finally responded:
Oh yes I see! Thanks for sending us that photo. Improvement in that atrophic skin are sometimes more stubborn but the CO2 laser is still thought to be the best solution. I would recommend continuing with CO2 laser treatment and the next time we do it we will take positional photographs and then map out each area of micro atrophy in detail so that I can consider applying potentially stronger settings to those areas.
The procedure notes I later requested follow (Figure 6). I was only instructed to return in one month for the next PRP treatment; no follow-up guidance was given in regard to the CO2 laser. I further argue returning in one month would not be adequate safety protocol for the CO2 laser in any case, as many doctors stress the importance of frequent (even daily) follow-up after ablative resurfacing procedures. Verma et al. write “Close follow-up during the initial post-procedure period to monitor for signs or symptoms of infection, pruritus, and other issues is imperative to reduce adverse outcomes and maximize the therapeutic benefit of ablative laser therapy” (Verma et al., 2022). Nikalji et al. write “Frequent post-operative visits should be done so that it can be ensured that appropriate home wound care is being performed and to minimize the risk of infection” (Nikalji et al., 2012). Ramsdell writes “In this series, every case [of scarring] was caused by infection, highlighting the need for surveillance, and proper skin care including possible antibiotic and antiviral prophylaxis” (Ramsdell, 2012b), none of which Dr. Wu provided me for this procedure. In addition, Dr. Wu was in and out for only as long as it took him to administer the treatment and gave me no opportunity to ask any questions. This altogether negates his account in the procedure notes stating “reasonable expectations discussed” and “Possible short and long-term effects were discussed to the patient’s satisfaction”.

Procedure notes for CO2 laser on my back, given to me after I had another doctor request them. I did not tolerate the procedure well, despite Dr. Wu’s notes, screaming in pain when Dr. Wu often lasered outside the well-numbed area.
🔗3.2. Pre-Op Concerns for CO2 Laser on My Face
I was convinced to do what Dr. Wu told me was the same procedure on my face too. There was a pre-op call this time with Dr. Wu’s nurse, Phyllis Massino (CALIFORNIA BOARD OF REGISTERED NURSING License 318808 License Type Registered Nurse)↗. She introduced the term prophylaxis without elaboration, and she gave me doxycycline 100 mg and Valtrex (unsure of dose) twice a day, both for ten days, starting one day pre-procedure. I expressed great concern over the doxycycline because I had been on it at least 3 times before for acne and it seemed like it stopped working in the later courses, but she said that since it had been more than a year since the last time I was on it, resistance was impossible since susceptibility bounces back. I also told her I was currently on sarecycline, another tetracycline-class antibiotic, long term for the past 1.5 years and that I had previously done minocycline (another tetracycline) twice as well, which I also felt I was resistant to. She still decided on doxycycline and did not give me another option. She said to start it 1 day before the procedure and continue it for 10 days, giving me only a 10-day supply. I question if she had the background to make the determination about whether I am resistant to an antibiotic and to decide what to prescribe, as she seemed to dismiss my concern about resistance. No susceptibility testing was offered either, despite having active lesions. Furthermore, doxycycline is not in one of the antibiotic classes (2- and 4-Quinolones, Cephalosporin, Macrolide, Penicillinase-Resistant penicillins, Lincosamides) doctors more typically prescribe as antibiotic prophylaxis for CO2 laser procedures (Horton & Alster, 1999) (Weinstein et al., 1997) (Christian et al., 2000) (P.R., M.D., in-person consultation, March 17, 2022.). According to other practitioners, doxycycline (as well as other tetracyclines) is contraindicated in CO2 laser resurfacing in particular due to its photosensitizing effect that can compound the already strong laser’s damage (“Laser Skin Resurfacing,” n.d.) (“Skin Care Before and After Fractionated Carbon Dioxide Laser Treatment,” n.d.). Sarecycline, which I once again alerted Dr. Wu and the nurse I was on long term up until the procedure, also carries a photosensitization warning↗ that they did not warn me about with respect to the CO2 laser.
I also alerted Phyllis that 3 months earlier, I had been on a high-dose course of prednisone at 60 mg per day for 8 days and had been left with adverse effects including tinnitus. At that dose for that duration and already having experienced other adverse effects, it was well within possibility it made me temporarily immunosuppressed, which could have multiplied my risk of infection for many months after (Youssef et al., 2016) (“Even Low Doses of Prednisolone Increases Risk of Infection,” n.d.). Horten and Alster add that “Because the thermal injury created by laser resurfacing is similar to a burn, localized immunosuppression occurs, which may predispose the patient to infection” (Horton & Alster, 1999). I think these risk factors were all the more reason for Dr. Wu to give me a more tailored antimicrobial prophylactic regimen (Metelitsa & Alster, 2010), not perform what I later found out was such an intense procedure on me, and/or monitor me and give me instruction on the possible complications and how to identify them.
I also alerted Phyllis I had latent tuberculosis, which I had also indicated on the intake forms when I first met Dr. Wu, and she told me an X-ray result confirming negativity for pulmonary tuberculosis from September 17, 2019 (1.5 years prior) was sufficient for safety. I also alerted her I was traveling from Mexico, and this prompted her to ask for a negative SARS-CoV-2 test, which I provided from January 26, 2021.
Phyllis now told me the procedure would be $4000 instead of the $3000 ($2500 for laser + $500 for subcision) they quoted me just over three months ago (Figures 1 & 3). I figured this was because the quote was only valid for 90 days, which had just passed.
🔗3.3. Being Coerced to Sign the Consent Form Under Duress
On the day of the CO2 laser procedure on my face, February 8, 2021, while I was waiting in the operating room (OR), Dr. Wu’s nurses gave me Percocet and Valium (they never disclosed the doses, and they did not record this in the medical records I later requested (Figure 8), but there are email records that they did give me these meds, but I will never know the doses). They had me wait while the drugs kicked in and made me loopy. After some time, the nurses gave the consent form to me and instructed me to sign it right then on the operating table. I was now under the influence of the incapacitating intoxicants the same nurses had administered me prior, and they kept rushing me to sign the form because the OR was booked after my slot. I therefore signed under duress without being given time or in the state of mind to possibly comprehend the form(s), and they never gave me a copy to fully read. I was denied my right to informed consent for the procedure, and whatever I signed documenting otherwise is null and void given these circumstances. Shah et al. write “The following are the required elements for documentation of the informed consent discussion: (1) the nature of the procedure, (2) the risks and benefits and the procedure, (3) reasonable alternatives, (4) risks and benefits of alternatives, and (5) assessment of the patient’s understanding of elements 1 through 4” (Shah et al., 2022). All 5 points were omitted or invalidated due to my inability to comprehend and consent in such a state of mind and under such pressure. Pandit and Pandit highlight the legal importance of informed consent in a section titled “What is Medical Negligence” that “unless it is an emergency, he [the doctor] obtains informed consent of the patient before proceeding with any major treatment, surgical operation, or even invasive investigation. Failure of a doctor and hospital to discharge this obligation is essentially a tortious liability” (Pandit & Pandit, 2009). The right thing to do in this case might have been to reschedule the procedure. I have discovered another person reporting similar treatment by Cosmetic Laser Dermatology, writing “The pages of CONSENT FORMS were given to me AFTER I was given a SEDATIVE.”↗
🔗3.4. Active Infection at the Procedure
I had waxing acne cysts on my right cheek, as can be seen in Figure 7 taken immediately before the procedure, and I made sure to ask Dr. Wu if it was still safe to perform the procedure before he began. He said they weren’t a problem and lasered over them indiscriminately. However, active infection, even just acne, is a nearly unanimous absolute contraindication in articles (Krupa Shankar et al., 2009) (Horton & Alster, 1999) (Yumeen & Khan, 2021) (Ramsdell, 2012a) (Verma et al., 2022) (“Skin Resurfacing - Laser Surgery,” 2021) (D. Apfelberg, 1997) and according to other doctors (J.P., M.D., in-person consultation, January 6, 2022.) because of the tendency for the procedure to cause the infection to spread, for one. The lesions should have been drained prior to performing the laser (J.P., M.D., in-person consultation, January 6, 2022.), at the very least. Alternatively, Dr. Wu could have marked and avoided them, though he made no markings for this procedure and did not get my approval or inform me on the boundaries he was going to laser within, which laser(s) he would use (he didn’t tell me the device name(s) or that he would use two laser heads), and what parameters (e.g., density and depth) he would use. Lastly, Dr. Wu could have given me the option at this point to reschedule the procedure.
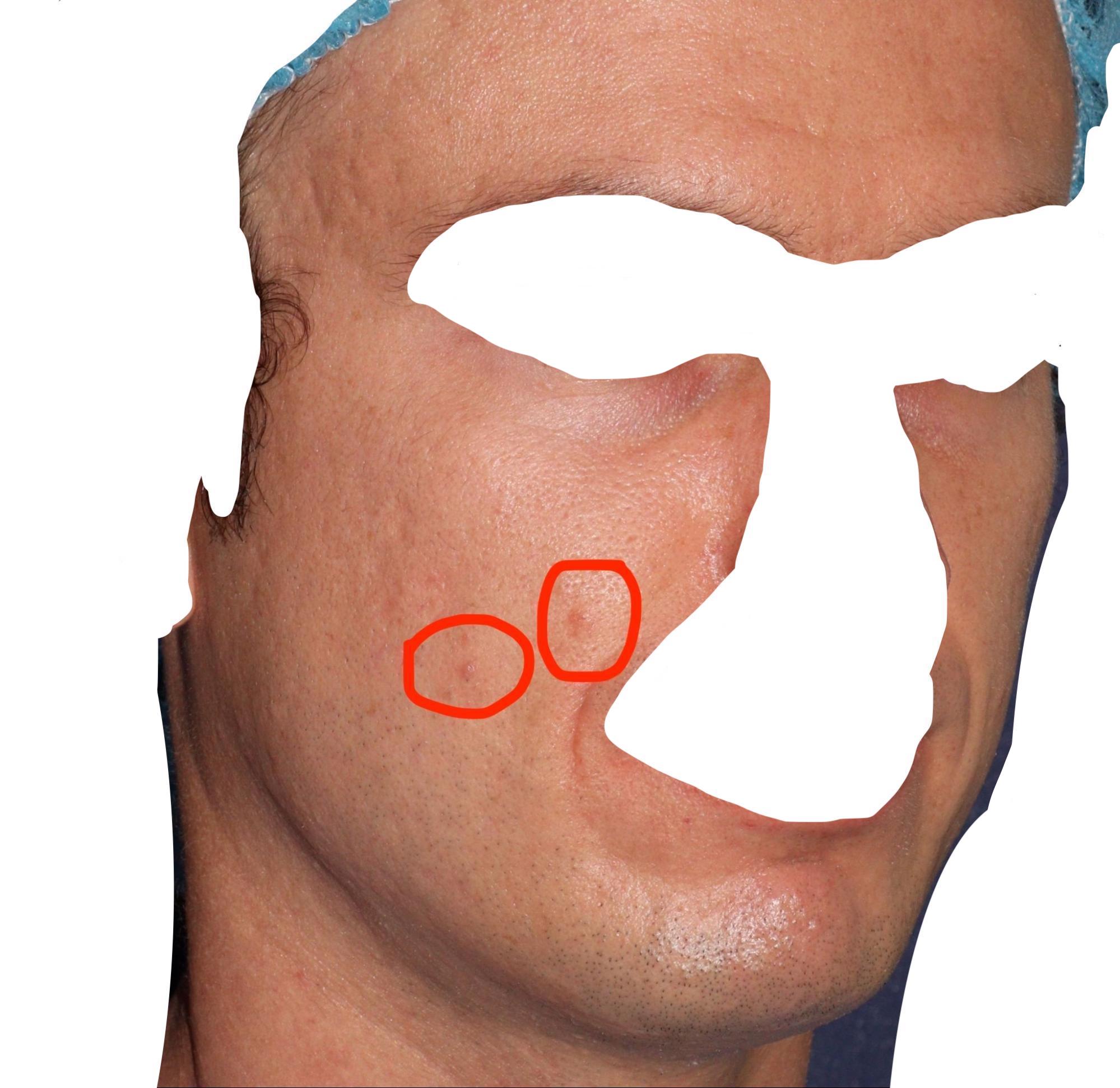
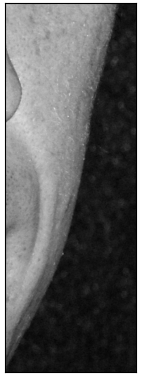
Photo taken by Dr. Wu’s office immediately before CO2 laser on Feb 8, ’21. 2 of the active acne cysts circled
🔗3.5. Misinforming Me on the Intensity and Type of Procedure
The two nurses (only one of which is documented in Dr. Wu’s notes from the procedure in Figure 8) who accompanied me and Dr. Wu in the operating room informed me prior to the procedure this laser would be of mild intensity on the range they perform. They seemed frantic after the procedure and rushed me out of the office when I was in distress about what to do and still out of it from the narcotics/sedatives they gave me. I asked the nurse guiding me to the exit for more post-op instructions but she insisted I leave and told me to ask the doctor any questions I had at our virtual follow-up the next day. I asked him during the follow-up why they told me it was going to be mild if it seemed so intense, and he said it was actually the most intense settings that there are for that procedure (Figure 12). I was taken aback because I couldn’t believe he would perform the strongest parameters for what I now know is the strongest laser available on the entire face when I had never had a laser on my face before. I also figured this could mean the most intense parameters are just not that strong because I had no understanding of the absolute range of intensity of laser treatments. I figured I simply had to follow the brief instructions Dr. Wu gave me, which only reiterated what (Figure 11) says about vinegar soaks and to apply Vaniply, and hope for the best. Months later when discussing complications with Dr. Wu, he changed his assessment again in an email on Jan 31, 2022 saying the procedure was performed at “moderate energy levels.” I had to get the procedure notes and ask other surgeons to find out the truth, which was that the procedure parameters were indeed intense.
Even with the oral and local pain medication, the laser on the face was far more painful than the laser Dr. Wu performed on my back previously. No additional pain management was provided despite demonstrating excruciating pain—Dr. Wu just kept telling me to hang in there a little longer. Little did I know that Dr. Wu also tuned this laser to be fully ablative (i.e., ablating 100% of the skin surface, plus possible overlap) unlike the one on my back that was fractionated (i.e., fractionally ablative), and he turned up the energy settings too. The quotes he gave me said they were the same treatment (Figures 1 & 2) and nobody from his office ever gave me an indication they would be different in any way. Dr. Wu and his staff always called both a fractional CO2 laser procedure. However, fractionated procedures are a world apart from fully ablative ones in terms of risk, with fully ablative ones carrying the most severe risks including hypopigmentation and full-field scarring (Preissig et al., 2012). Fractionally ablative laser utilizes the principle of fractional photothermolysis, in which the areas of untouched skin among the treated areas enable faster tissue proliferation aimed at repairing the damaged zones (Marqa & Mordon, 2014). Fully ablative laser completely loses out on this and fully exposes the dermis to all possible complications (da Cunha et al., 2015). I would have never done the laser if Dr. Wu had informed me of these aspects of the procedure and the potential complications. The procedure notes follow (Figure 8). The parameters described in the section labeled “UPCO2” are for the Active FX, as Dr. Wu later informed me. The density Dr. Wu used for the Active FX is 6 (indicated by the pattern-size-density note of 3-9-6), which is fully ablative (plus potential overlap) (Al-Niaimi, 2015) (Ramsdell, 2012a). Dr. Wu had informed me before the procedure that the procedure would be fractionated. I inquired 7 months post about what the laser settings meant and Dr. Wu emailed me back Sep 2, 2021 saying,
A laser density of 10 with this particular laser means that 10% of the skin surface area was treated by direct laser beam. The entire point of fractional laser is to treat a percentage of the skin while leaving a percentage untreated so as to promote the best possible healing response. In my opinion, your healing is not abnormal and I do believe that there will be consistent and continued improvements in your skin moving forward.
His response only covered the Deep FX portion of the treatment, so I responded 3 times asking about the density of the Active FX portion, to which Dr. Wu never responded. I wonder if he even knew the settings he used with that laser are fully ablative considering his prior response explaining his intention to only treat a percentage of the skin surface.
Furthermore, Dr. Wu recorded the spot size for the Deep FX as 10 mm. However, that is not a possible spot size to my knowledge and leaves me to wonder what the actual spot size was, which is relevant in calculating the fluence and power density of the procedure using the device manual. This also brings to question the accuracy of the rest of this medical record, which is important in assessing if safe energy settings were applied.
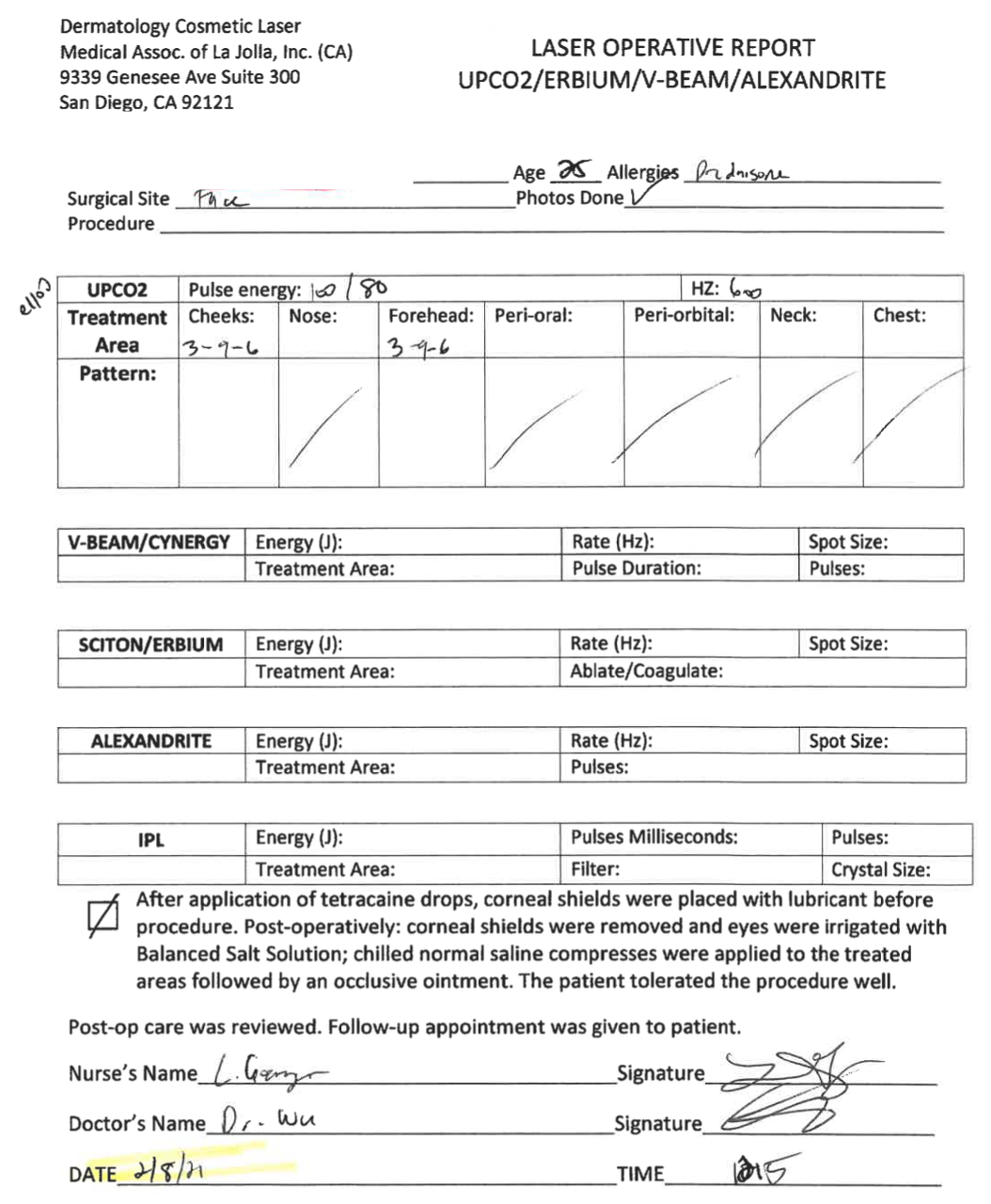 | 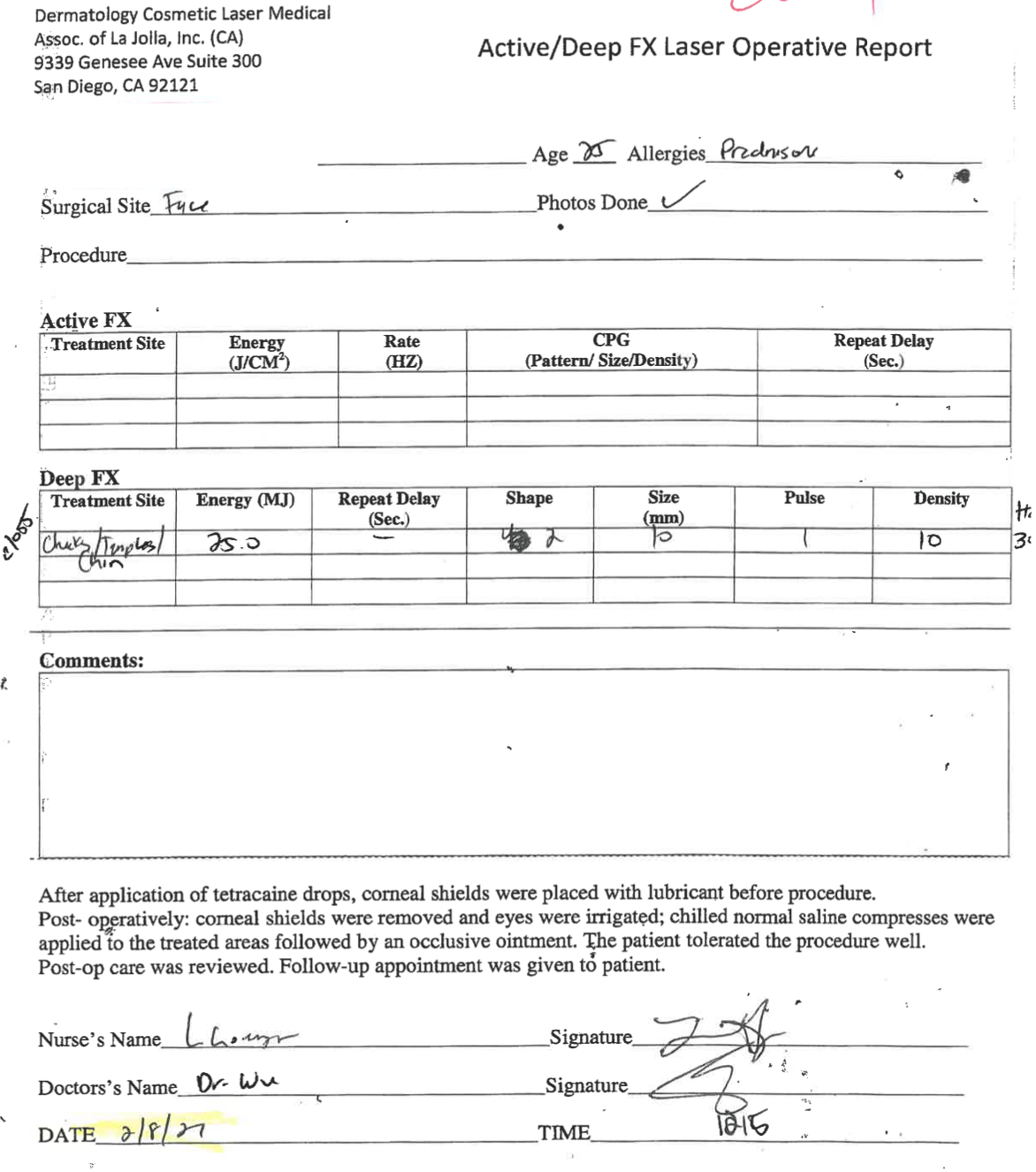 |
Procedure notes for CO2 laser on my face, given to me after I had another doctor request them.
I also want to address that Dr. Wu informed me by email Oct 13, 2020 that he would blend the edges of the treatment area to minimize any chance of telling the treated area apart from the untreated. However, I did not observe this effort taken, as he only noted changing the Active FX pulse energy from 100 mJ to 80 mJ (Figure 8). Other doctors (Ramsdell, 2012a) also lower the density to feather, in addition to manipulating the handpiece to fire tangentially, and I would think such parts of the treatment would be noted if they were done. This resulted in stark delineations between some treated and untreated areas (Figure 9), which became even more pronounced after healing by the complications I experienced in the treated area (Figures 30, 32, 37.B, 39).

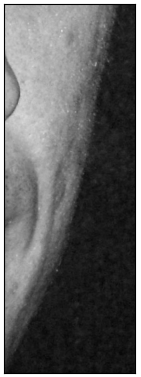
Feb 12, ’21, 4 days post. Sharp delineation in circled area
🔗3.6. Safety Protocols at the Procedure
In anticipation of the first pulse, I did not hear Dr. Wu fire the laser before using it on me in order to preview the laser patterns or check the alignment of the laser beams, which I believe is typically done by firing the laser onto a wooden tongue depressor before beginning treatment. The advice in the device manual↗ (p57) warns:
CAUTION - Before beginning a procedure with the UltraScan Encore CPG or the SurgiTouch scanner or the DeepFX microscanner, always preview the pattern. Repeat the pattern preview instructions during treatment if the pattern is changed, if single exposure is changed to timed exposure, or if the time delay between patterns is adjusted. Delivering the treatment beam to the target tissue before previewing the pattern may result in unintended laser-tissue interaction.
CPG (computerized pattern generator) seems to be synonymous with Active FX↗. With regard to the laser-beam alignment, the manual↗ (p31) warns:
WARNING - Beam alignment checks are extremely important for the safe operation of your laser equipment. Do not use the laser or delivery system if aiming and treatment beams are not coincident; call your local Lumenis representative. Misalignment of aiming and treatment beams may result in laser exposure to nontarget tissues and possible injury.
However, Dr. Wu targeted 3 of the hypertrophic scars that I indicated were caused by RF microneedling, and I emailed him and his assistant 3 months post to say it seemed like he missed 2 of the 3 (i.e., hit beside them). I explained “I remember immediately after it seemed like Dr [Wu] hit the chin spot perfectly but it seemed like the two others were not hit but instead the spot laser hit beside them. And that seems to me consistent with how they appear now: I think the chin one improved 80% but the other two did not.” This adds to my concern about forgone alignment protocols.
Furthermore, no tetracaine drops and corneal shields were placed even though the notes have the box next to that marked on the first page and state it as fact on the second page (Figure 8); solely ill-fitting goggles were used, which worried me during the procedure and which I questioned Dr. Wu about prior to beginning. He assured me it was safe and gave no alternative, but it seems corneal shields would have been safer, especially because this was a high-fluence, long-wavelength procedure that got within centimeters of my eyes (Huang et al., 2018). Also note that both items about the corneal shields in the notes are followed by “The patient tolerated the procedure well”, which seems odd to presuppose and makes me wonder how much of all my notes are generated from templates not according to the actual care I received.
Lastly, no skin cooling (e.g., contact or Zimmer cryogenic cooling) was given on the area being treated aside from whatever the UltraPulse device provides, which seems to depend on if Dr. Wu connected the optional purge air compressor for both the Deep FX and Active FX heads↗ (p13). Huang et al. write “Inadequate cooling between pulses also predisposes to injury by cosmetic lasers” (Huang et al., 2018). No cooling was offered immediately after either, perhaps because I was forcibly rushed out of the office.
On another occasion when Dr. Wu was performing a session of PRP scalp injections, his nurse dropped syringes of my PRP on the ground, contaminating the sterile field (Tennant K, 2021). The nurse proceeded like nothing happened, setting them on the table for Dr. Wu who subsequently used them on me without any resterilization. I did not speak up because I did not know the dangers of this and expected that they were well trained. In addition, at another one of my PRP treatments, the centrifuge, which was in the same room as me, began to rattle and smoke while it was processing my blood. A nurse came in and stopped it, and observed the blood appeared separated even though the full processing time hadn’t elapsed and told me it was good, completely disregarding that the appropriate platelet concentration obviously wasn’t reached.
🔗3.7. Questionable Laser Settings
I suspect excessive laser energy was delivered to the mandible ridge area, where Dr. Wu performed the Deep FX at 25 mJ (Figures 8 & 10). Ramsdell writes in regard to the Deep FX, “At 22.5 mJ, ablation extends to ∼675 μm, which correlates with deep dermis (depending on skin thickness)” (Ramsdell, 2012a). Linearly extrapolating to 25 mJ gives an ablation depth of ∼750 μm, and this does not account for the residual thermal damage CO2 lasers in particular are known to deliver beyond the area of ablation. The mandible skin is thinner than other areas, so it seems the laser may have ablated excessively deep. Furthermore, the mandible is particularly prone to hypertrophic scarring after injury/resurfacing due to the relatively high skin tension in the area (R.J., M.D., in-person consultation, March 30, 2022. & P.R., M.D., in-person consultation, September 1, 2022.), which would also warrant more conservative settings in that area (Metelitsa & Alster, 2010). Saedi et al. warn of this in regard to fractional photothermolysis in writing “The periorbital and mandibular ridge can also be scar prone and should be treated with more conservative parameters” (Saedi et al., 2012). Horton and Alster reiterate this: “Moreover, certain facial areas are prone to scar formation, such as the philtrum, infraorbit, mandible, and neck. Extreme caution should be exercised when determining the laser settings and number of laser passes in these areas” (Horton & Alster, 1999). Gauglitz writes the same about wounds in general: “Wounds subjected to tension due to motion, body location, or loss of tissue are at increased risk of scar hypertrophy and spreading, and patients should be informed of this important matter prior to any surgery” (Gauglitz, 2013). Yet Dr. Wu did not inform me of this and didn’t so much as use a diagnostic tool to measure skin thickness before applying the same or stronger settings (for both the Deep FX and Active FX) over scar-prone areas and the rest of the face alike.
 |  |
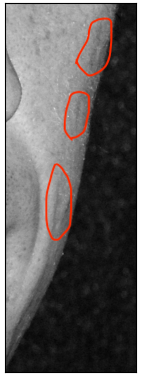
Feb 12, ’21, 4 days post, circled areas showing where the Deep FX was applied
With regard to the Active FX Dr. Wu performed over the entire face, he did not seem to assess vellus hair/skin-adnexal–structure density in the areas he planned to fully ablate (“Skin Resurfacing - Laser Surgery,” 2021), which could have been done with dermoscopy. Hair follicles are the primary source of epidermal keratinocytes that repopulate the area after full ablation (Sun et al., 2022) (R.J., M.D., in-person consultation, July 14, 2022. & P.R., M.D., in-person treatment, August 10, 2022). Dr. Wu had diagnosed me with a form of alopecia without confirming the type via standard diagnostics (Section 1), he was treating post-inflammatory scars, and I had reported scarring from RF microneedling. These were all reasons my skin may not have had the hair-follicle density needed to safely regenerate after full ablation in some areas, and it would have been prudent to confirm adequate density before full ablation, start with less extreme settings, and/or conduct a test spot.
🔗3.8. Post-op Instructions
Pretty much the only post-op instructions given to me were to do dilute-vinegar soaks every few hours until the crusts came off (I was not told when to expect the crusting to resolve), reapply Vaniply, and take the doxycycline and Valtrex for 10 days total. I was not educated on the importance of avoiding double-dipping in the dilute vinegar to prevent infection risk (Christian et al., 2000). There were no warnings about infection due to the procedure or other safety instructions given to me. Figure 11 shows the complete instructions the pre-op nurse emailed me. Despite saying there are additional instructions for the rest of the face, none were given to me (Nurse Phyllis Massino, email, January 26, 2021.), and I thought nothing of it since, once again, I was led to believe this was going to be a safe procedure exactly the same as the one I had previously received from him on my back, for which no written instructions were given.

Full post-op instructions emailed to me Jan 26, ’21 by Dr. Wu’s pre-op nurse, Phyllis Massino
Dr. Wu had a few-minute follow-up with me the morning after over video (Dr. Wu preferred I not come in, presumably to minimize COVID-19 transmission risk). Once again, pretty much all he advised was to do the soaks and keep the area moist with Vaniply ointment. The instructions (Figure 11) just say “Apply ointment to the areas with clean fingertips”, but I also feel this part should have been more detailed to specify that too much ointment can “enhance the likelihood of pathogen overgrowth” (Metelitsa & Alster, 2010), as Nikalji et al. write “Avoid occlusive dressing in the immediate post-operative period because of its propensity to promote folliculitis and streptococcal and staphylococcal infections” (Nikalji et al., 2012). I even emailed Dr. Wu 16 days post with concerns that I applied too much ointment and was worried about it “becoming a petri dish since I doubt the soaks can penetrate that level of thickness”. He only told me to try soaking it off over email and offered no further help.
Dr. Wu left off the call saying to email him, not call him, if I had any questions, and I respected his preferred communication channel and only emailed, never calling his emergency phone number, which was given to me this time. No other follow-up appointment was offered to me, and he booked out weeks, so any chance to see him again regarding this procedure seemed slim. However, I didn’t think there would be any need to see him again because he never gave me follow-ups for any other procedures (including what I thought was the same procedure on my back). No instructions to send him photos periodically were given to me, whereas other doctors advise it is imperative to monitor the patient closely in the acute healing phase pre-re-epithelialization (Ramsdell, 2012b) (Verma et al., 2022) (Nikalji et al., 2012). Note that Dr. Wu’s records from our appointment (Figure 12) (which were not given to me until another doctor made a records request months later) claim he discussed “blisters” (which are different from papules, pustules, and nodules), “signs of illness”, sending photos, and that I could schedule an appointment at any time, but I categorically refute that. I back this up in asking why I would not at least be given these critical instructions before the procedure instead of the morning after a terrible night of sleep in pain due to the procedure only by voice. This exact same note is, however, correct in saying “What to expect/Post op Instructions given No”. Verma et al. educate that “Patients should be informed of the expected recovery timeframe and regularly monitored by the interprofessional healthcare team to ensure normal healing” (Verma et al., 2022). Yumeen et al. elaborate on the importance of these in writing “Infectious complications, including herpes simplex virus reactivation, and bacterial and fungal infections, can impair healing, and appropriate prophylaxis should be administered. Patients should be followed carefully after treatment to provide clinicians the opportunity to identify and promptly manage any complications that may arise” (Yumeen & Khan, 2021).

Notes from virtual follow-up 1 day post, given to me after another doctor requested them
Dr. Wu performing a completely different procedure from the one I thought I signed up for, along with a lack of post-care guidance and inattentiveness led to major complications that went unrecognized, despite me reaching out for help many times (Section 4). Also note that Figure 12 says the CO2 resurfacing excluded submental on the 4th line, but then indicates on the 7th line that the submental was treated. Lastly, note that on the 4th line it says the laser used was the Scar FX, which seems like a mispelling of the SCAAR FX; however, in other notes like Figure 16 it says the Active/Deep FX (which comprise the Total FX) were used. These are completely different treatment modes↗ and leave me wondering what I actually got.
🔗4. Post-Procedure Issues
🔗4.1. Dismissing Segmental Delayed Healing
I initially emailed Dr. Wu and Cecelia 8 days post (as they hadn’t reached out to me like I thought they might) to update that I felt I was 80% peeled. However, I emailed Dr. Wu with photos (Figure 13) 16 days post, expressing concern over my jawline still having scabs (i.e., delayed healing, which I later learned is a major concern) and that it was “becoming a petri dish since I doubt the soaks can penetrate that level of thickness”. But he responded “Got it. I don’t think there’s any major cause for concern. Perhaps try soaking it off a few times a day? In general, I’d rather you not rip or peel the scabs off.” When I emailed two days later telling him I was worried because I had an expectation of this stage lasting 10 days and that it still hadn’t healed after nearly twice as long at this point (18 days), he did not respond to that part of my email but instead just responded to the part where I also asked for an acne antibiotic (because I was breaking out), approving my request to prescribe sarecycline, a narrow-spectrum tetracycline-derived antibiotic whose activity is limited to mainly Cutibacterium acnes, without confirming my lesions were susceptible to it. This is questionable in general but especially dubious immediately after a procedure that opens the patient up to a vast variety of infection types and due to Dr. Wu knowing I was on sarecycline long term immediately prior to the procedure, which would also introduce the concern of resistance, especially since the drug’s efficacy has not been tested beyond 6 months. He assured me everything was normal without offering to see me in person or even asking more questions, so I figured I was being dramatic. However, re-epithelialization should only take 7-14 days (Horton & Alster, 1999) and delay beyond that often indicates complication like infection (Nikalji et al., 2012) (Metelitsa & Alster, 2010) (A.B., M.D., in-person consultation, March 8, 2022.). Ramsdell writes “The most common cause of scarring is postoperative infection, which usually presents several days postoperatively as a localized area of delayed healing” (Ramsdell, 2012b). Gauglitz echoes this, writing “Delayed epithelialization beyond 10–14 days is known to increase the incidence of hypertrophic scarring dramatically thus achievement of rapid epithelialization is mandatory for avoiding excessive scar formation” (Gauglitz, 2013). Furthermore, the antiviral at the very least should be taken up until re-epithelialization (Weinstein et al., 1997) (Horton & Alster, 1999), but of course the 10-day supply Dr. Wu prescribed had run out and he did not address this. I believe the same goes for the antibiotic. The scabbing ultimately resolved at 21 days post.
 |  |  |
The photos I took and emailed Dr. Wu for evaluation on Feb 24, ’21, 16 days post, showing unresolved scabbing throughout the beard.
🔗4.2. Not Seeing Me in a Timely Manner with Post-op Concerns
On March 5, 2021, less than a month post, I emailed Dr. Wu and his assistant, Cecelia, about significant redness inquiring “how much longer I can expect to be significantly red. I remember that Dr. Wu has said the longer the redness lasts, the better the result, but I’d just like an idea of what more I’m in store for and if there’s anything else that might help such as bleaching cream.” Cecelia responded, without asking any questions or for photos, that they could look at my skin regarding my concerns about redness at my next PRP appointment with Dr. Wu. However, when I tried to schedule an appointment for the week of March 22nd, 2021 (Dr. Wu told me PRP needed to be done on a strict schedule, and that was when I was due for the next one), Dr. Wu was out and Cecelia said I needed to wait until his next availability April 12th, even though there were six other doctors at his practice and many other staff who should be equipped to handle these concerns, including Dr. Wu’s own assistant. Cecelia was confident in telling me March 5, 2021 over email: “At this point in your recovery, though, there is nothing we recommend adding in to expedite its demise. Post-resurfacing redness is one of those ‘time heals all wounds’ scenarios where it will dissipate over time as you continue to heal.” However, redness—depending on the severity, coexisting symptoms, and evenness—can be good or bad at that stage, and her blanket answer completely assuring me of normalcy did not cover the cases where it might indicate infection, contact dermatitis, and/or incoming scarring (Metelitsa & Alster, 2010), and neither she nor Dr. Wu further assessed. Horton and Alster (Horton & Alster, 1999) explain “Prolonged or excessive erythema may be due to superficial infection or contact dermatitis.” Ramsdell educates “Candidiasis may be quite subtle and present as prolonged erythema and pruritus. Herpes simplex virus may disseminate over the entire face without prophylaxis. Atypical mycobacterial infection has also been reported and may present as papules or nodules” (Ramsdell, 2012b). I also had pruritus persisting beyond re-epithelialization in some areas, but the nurses had told me itching was expected throughout healing (which Dr. Wu had told me takes 6 months) and to just take Benadryl® if it bothered me. In addition, Dr. Wu always told me that more inflammation meant better results without ever counseling me on the nuances. I also had pustules and cysts present, but I thought it was acne, which Dr. Wu affirmed several times without culturing. I mentioned in the same email March 5, 2021, “My deepest scars have lifted noticeably and I hope that being a month in means that is permanent and there is more to come.” However, this perceptible improvement was likely impossible for less than a month out and actually might have indicated worrisome edema, which I now know is common alongside an infection.
🔗4.3. Signs of Contact Dermatitis
On March 31, 2021, I emailed Dr. Wu and his assistant, Cecelia, that I had begun using a topical retinoid, Tazorac .05% cream in particular, as Dr. Wu instructed me to do after re-epithelialization but that I needed help. I wrote “Would you prescribe me Tazorac .025% Cream? I have been using the .05% but it is too strong now and my skin has been peeling because of it.” Awaiting the prescription, I followed up a couple days later saying “I’ve just been been applying moisturizer before the tazorac in the meantime and have noticed the peeling subside.” Cecelia responded “I just spoke with the CVS pharmacists this morning and I guess Tazorac does not come in 0.025% and the lowest dose they have is the 0.05% that you are already using. It sounds like perhaps the irritation has passed, you’re doing exactly the right thing by incorporating moisturizer when you apply the Tazorac.” However, Ramsdell (Ramsdell, 2012b) advises a product suspected of causing contact dermatitis, which can be irritant or allergic in nature, should be discontinued immediately, not just buffered as I was advised. Furthermore, once contact dermatitis has occurred, it is important to treat the potentially precipitating inflammation with a topical corticosteroid to prevent scarring, which Dr. Wu never advised. Roberts et al. affirm this in part in writing “If an allergic dermatitis is suspected, the topical agent should be stopped and treatment begun with a strong steroid cream” (Robertsiii et al., 1996). Dr. Wu never offered me a steroid cream.
🔗4.4. More Signs of Contact Dermatitis and Infection
I wrote Dr. Wu and Cecelia again Apr 5, 2021 (almost 2 months post, before the first in-person follow-up) expressing concern over a glossy/shiny look my skin now had. I said “whereas I could previously slide my finger across it, my finger now grips onto the sticky skin. I’ve seen others online describe it as orange peel and of course their stories of this being permanent worry me.” I asked if using a retinoid (as Dr. Wu suggested to enhance results) was best in this case. He responded “this doesn’t sound abnormal to me but please send us some photos of your skin so I can double check”. I sent Dr. Wu and Cecelia two emails in response with 3 photos (Figure 14) showing active cystic lesions; swollen, patchily red skin; and irregular texture, and neither Dr. Wu nor Cecelia responded to either email.
 |  |  |
The 3 photos I sent in 2 separate email responses to Dr. Wu and his assistant, Cecelia, Apr 5, ’21, almost 2 months post. Active cystic lesions around the mouth, beard, and nose; significant inflammation causing the skin to hypertrophy around the pores; and patchily red skin noticeable
🔗4.5. Infection Symptoms In Office
When I visited Dr. Wu’s office for the first time after the procedure, over 2 months post, the front desk advised that I had a fever when they checked my temperature. Dr. Wu’s staff did not think anything of it—they didn’t even note my temperature in my medical records like they usually did (Figure 16). They suspected the thermometer was faulty, so I didn’t think much of it either. I alerted them I had also gotten my first COVID-19 vaccination that day and thought that might have caused the fever. I had no idea at this point that fever could be a symptom of a skin infection (Christian et al., 2000). Dr. Wu looked at my skin, which had active cysts and was inflamed, and told me I was healing great. He did not have time for me to take off my sunscreen to show him better, but there were plenty of worrying symptoms visible that should have been of concern, as can be seen in the photos his office took of me (Figure 15). I told him I was worried about this irregular waxy, bumpy texture that developed as well as seeming fat/volume loss after the laser (Figure 16), but Dr. Wu said it was normal and would get better. He now advised purchasing TNS Recovery Complex from his office to use twice a day to help my concerns (Figure 16). He said acne was common after laser and that the sarecycline and topical retinoid would help if I gave those medications more time to work. He did not ever make me aware of the option to test the pustules or that I might have an infection. Ramsdell writes “Inexperienced or inattentive surgeons as well as patients may find it difficult to distinguish infection from the normal healing process. When an infection is suspected, it is advised to promptly perform microbiologic culture testing to identify the organism and determine its sensitivity to treatment” (Ramsdell, 2012b). Prohaska et al. reinforce this, writing “Postoperative infections, on the other hand, can be very difficult to diagnose as the typical appearance of the skin is disrupted from baseline. This presents the clinician with the difficult task of differentiating cutaneous infection from burns or normal wound healing. A culture can be very helpful in the diagnosis” (Prohaska & Hohman, 2022). I did not even realize infection was possible at this point nor did I know what it would look like, as this was the first laser and ablative procedure I ever had on my face—as well as my first fully ablative treatment, which I still wasn’t aware of at that point—and Dr. Wu never warned me about the possibility of infection and what it would look like. In addition, I was used to getting hormonal cystic acne and didn’t know lesions could be anything else. The infection could have been delayed onset, which has been well documented (Christian et al., 2000), or just continuing from immediately post CO2 laser, signaled by the delayed healing, breakouts, and irritation I started getting about 2 weeks post, all of which I alerted Dr. Wu and his assistant about multiple times and either got told everything was normal or didn’t get any response.
 |  |
Apr 12, ’21, 2 months post, photos Dr. Wu’s staff took at my first in-person follow-up post-laser showing cystic lesions throughout the lower face and texture I raised concern about to Dr. Wu. Erythematous patches show through but are largely hidden under sunscreen.

Notes from first in-person follow-up over 2 months post CO2 laser
🔗4.6. Selling Me Other Treatments
When I emailed Dr. Wu three months post to say “my skin texture still seems abnormal to me (overly glossy, more textured than I remember, and seemingly impervious to topicals)” and that I was still red, he only responded “Persistent erythema at this point is not uncommon - sorry for the inconvenience, but if it’s continuing to trend in the right direction then everything is on track.” However, Horton and Alston (Horton & Alster, 1999) warn “Prolonged erythema that cannot be explained by other factors, and its association with tissue induration, herald incipient scarring.” Induration is when soft tissue, especially the skin, becomes thicker and harder due to an inflammatory process caused by various triggering factors, and this is exactly what I believe I was describing in as much detail as I could without knowing what it was at the time.
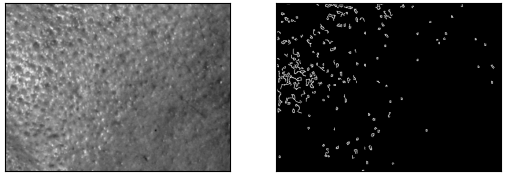
In that same email, I also asked about further subcision since I had only seen worsening in my original scarring, and Dr. Wu very oddly insinuated I now had ice-pick scarring, writing “Pitted ice pick scars typically do not respond to subcision that well. We can discuss further at your next appointment.” However, I had tried showing him that my skin was highly inflamed and swelling around the pores post CO2 laser multiple times, and he had previously mainly treated me for rolling scars (Section 1) and had of course performed two subcisions, which are “mainly useful for rolling scars (distensible, depressed scars with gentle sloping edges)” (Chandrashekar & Nandini, 2010). I emailed back trying to clarify my concerns: “I’m attaching a couple photos of my bare skin this week for your consideration. I think I was able to capture some of the textural irregularity I mentioned previously to hopefully give you more to go on. In the second photo I crease my skin in order to exaggerate these creases that I feel aren’t normal.”
 |  |
Photos I emailed Dr. Wu May 10, ’21, 3 months post, highlighting signs of induration, an increase in the fibrous elements in tissue commonly associated with inflammation and marked by loss of elasticity and pliability.
His new assistant, Brittany Enriquez, emailed me back saying “Dr. Wu chatted with me today. After reviewing your photos, he does recommend adding Vbeam laser to the current laser recommendations. He wanted me to include that the Vbeam laser will not inhibit collagen formation. The price for the Vbeam for the face is $500.00 per treatment.” I now know what I really needed at the time was something to inhibit the overgrowth of collagen. I did that as he suggested, even though I thought his office originally told me any further treatments related to the CO2 laser would be included. I specifically told him the bottom edge of the treated area was the most irritated but he did not adequately treat it, so the iatrogenic scarring ended up worse there. I emailed him and Brittany June 14 after he performed the Vbeam® vascular laser asking if a second session would be needed because I was still red, and neither he nor Brittany responded. I emailed him and Brittany again June 27 and he responded that time saying he recommended a second vascular laser session 2 months after the first, which I did as well.
I emailed Dr. Wu again July 14, 2021 reiterating my concerns about texture:
The redness is actually not bothering me as much as the irregular texture of my skin where I had the laser. I think it may be what is known as orange peel skin. I want to attach a photo from today that shows it well. Do I just need to wait longer for this to resolve (is it caused by some sort of microswelling from the inflamation [sic] from the energy or is it perhaps abnormal pockets of growth?) or is there some procedure that can help with it? Is my retinoid potentially causing it? I’ve had people comment on it and I’m really getting in my head about it. I bring it up because I’m not sure if I was ever able to clearly demonstrate what I meant and therefore get some sort of plan from you.
I attached the following photo (Figure 18).

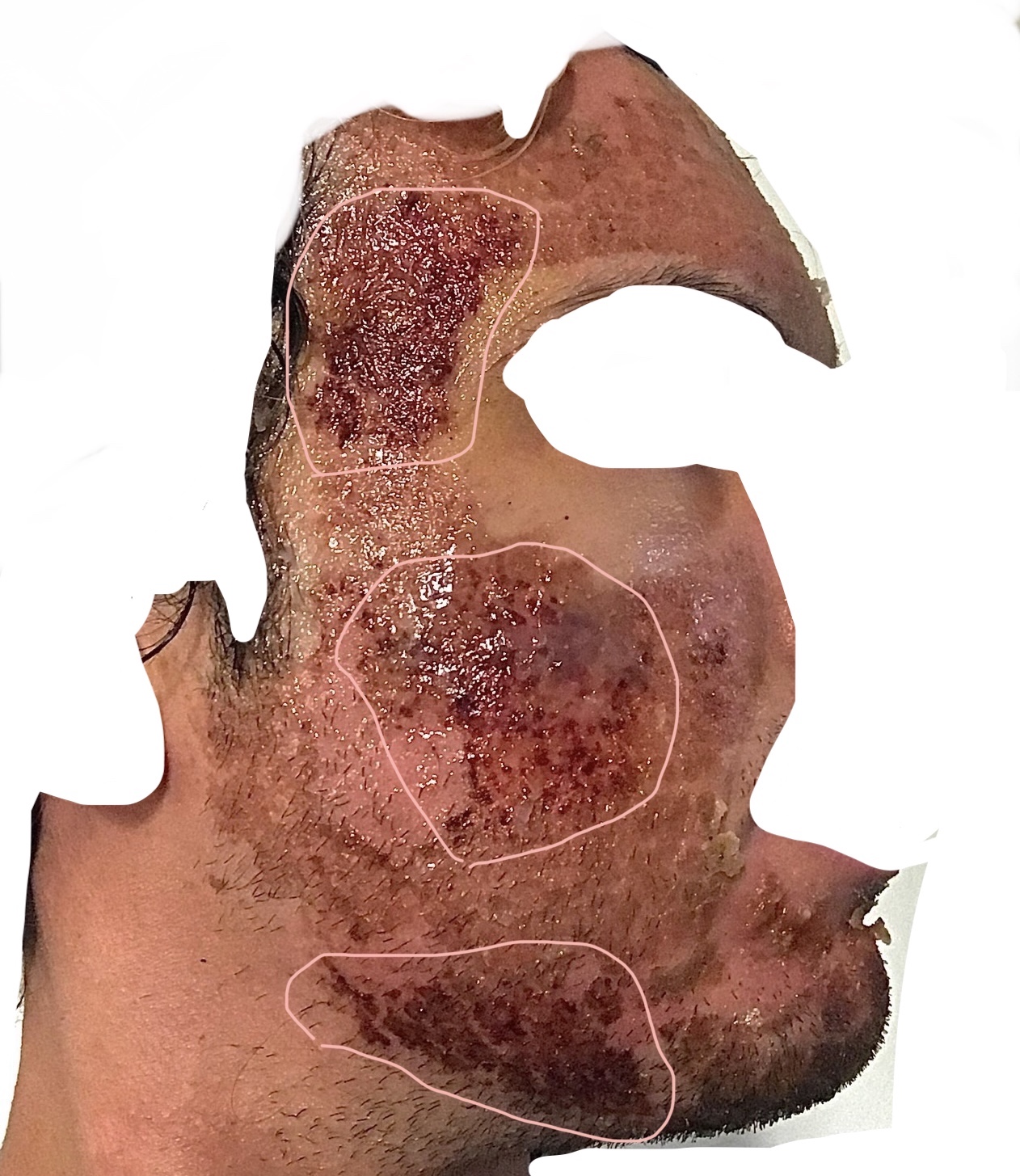
Photo I emailed Dr. Wu July 18, ’21, 5 months post, showing hypertrophic scarring throughout the entire treated area
He responded questioning my observations, recommending more treatments, and attaching a select pair of photos (Figures 19 & 20) out of the ones his office had taken that didn’t show the problem as clearly. His response was:
I’m sorry this has been a persistent problem. I acknowledge that this is bothering you and hope I’m not giving the impression that I’m taking it lightly. I’ve attached your most recent pics taken in my clinic under controlled conditions so that we can compare your baseline to back when I last saw you in June. To my eye, other than the mild persistent redness, there appear to be noticeable improvements in skin quality. I’m absolutely not disputing what you’re experiencing - just want to get to the bottom of things. I could be missing something or mistaken in my assessment. Perhaps you can evaluate them and tell me what you see? In regards to solutions to the problem, yes the first thing I’d recommend at this point is to discontinue the retinoid or any other micro-irritants that you may be currently using topically. It’s possible these are contributing to what you are experiencing.
Would you say the situation is getting better, worse, or staying the same? We are approaching the six month mark whereby most of the laser effects have typically run their course, although in truth cellular and molecular changes can continue even beyond that time point. But if things are trending towards improvement, then I think we can continue to wait. However, if you think that things have plateau’d, then there are milder laser and/or RF microneedling options that may be appropriate for you at this time. These treatments are designed to improve skin texture and were originally potential options for you moving forward after the initial laser procedure that we did.
We’ll sort this out for you [MY NAME]. Thanks for your patience and continued trust in my care.
I found it extremely odd he was now recommending RF microneedling after initially telling me I was not a candidate (Section 1). Out of all of these new things he started recommending, he still never gave me the option of a topical corticosteroid.
Photos Dr. Wu’s office took that Dr. Wu relied upon diagnostically A. Feb 8, ’21, immediately pre-procedure B. Jun 1, ’21, almost 4 months post
Photos Dr. Wu’s office took that Dr. Wu relied upon diagnostically A. Feb 8, ’21, immediately pre-procedure B. Jun 1, ’21, almost 4 months post
I responded:
Thank you for the more thorough response and guidance than before.
Firstly, I appreciate you sending the photos for my evaluation. I admit it is hard to see any deterioration therein. I think I see a slight difference in camera focus between each but luckily the “before” seems to be the one better focused in the region of interest (I’d say I primarily see this concern across my lower cheeks / the beard area). I discern this difference in focus from the clarity of the beard follicles.
I would say the situation is staying the same (I’ve discontinued the retinoid). I’m sorry I haven’t given you more to work with here. Please allow me to show you two higher-quality photos that illustrate my concern. You can see the skin is split up into little protruding globules. You can see that all through the beard area but also outside it, I believe. The outlined areas just show where I thought it looked clearest in the photos.
I attached these photos (Figure 21):
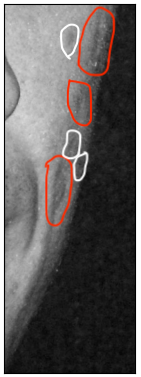
 |  |
Photos I took and sent to Dr. Wu Jul 19, ’21. Red areas highlight where the scarring is most visible, but it extends the whole treatment area
Once again, just when it seemed like Dr. Wu was beginning to take me seriously, he never responded. I argue that in my descriptions and photos I shared with Dr. Wu in Sections 4.4, 4.5, and 4.6, I consistently demonstrated three complications listed with their treatment in the device manual↗ (p147): “induration that generally resolves over time with steroid treatment”, “formation of fibrotic tissue that generally resolves over time with steroid treatment”, and “scarring that generally resolves over time with steroid treatment”. Yet Dr. Wu never once informed me of the option of a corticosteroid to treat my symptoms. In a sample of 174 medical malpractice claims relating to laser injury, Jalian et al. (Jalian et al., 2013) find that “notable allegations included failure to conduct a test spot (n = 17), failure to recognize and treat injury (n = 10), and failure to evaluate skin type (n = 7).” At this point, I believe I had experienced all of these, among others, multiple times.
🔗4.7. Diagnostics
I contested the “controlled conditions” (Section 4.6) under which the photos (Figures 19 & 20) Dr. Wu used to assess my case were taken and tried my absolute best to show him my symptoms many times with descriptions, with photos, and in person when he made time for me, but he did not seem to listen or respond. Dr. Wu’s staff did not allow me to take off my sunscreen for the “after” photos, and the focal points of the images differ (making the areas of concern blurrier in the “after” photos). Disregarding these inconsistencies, these photos do not support Dr. Wu’s claim that there are “noticeable improvements in skin quality” (similar to the situation in Section 3.1 where he claimed he saw noticeable improvement on my back), and they actually show the opposite, including some of the concerns I voiced.
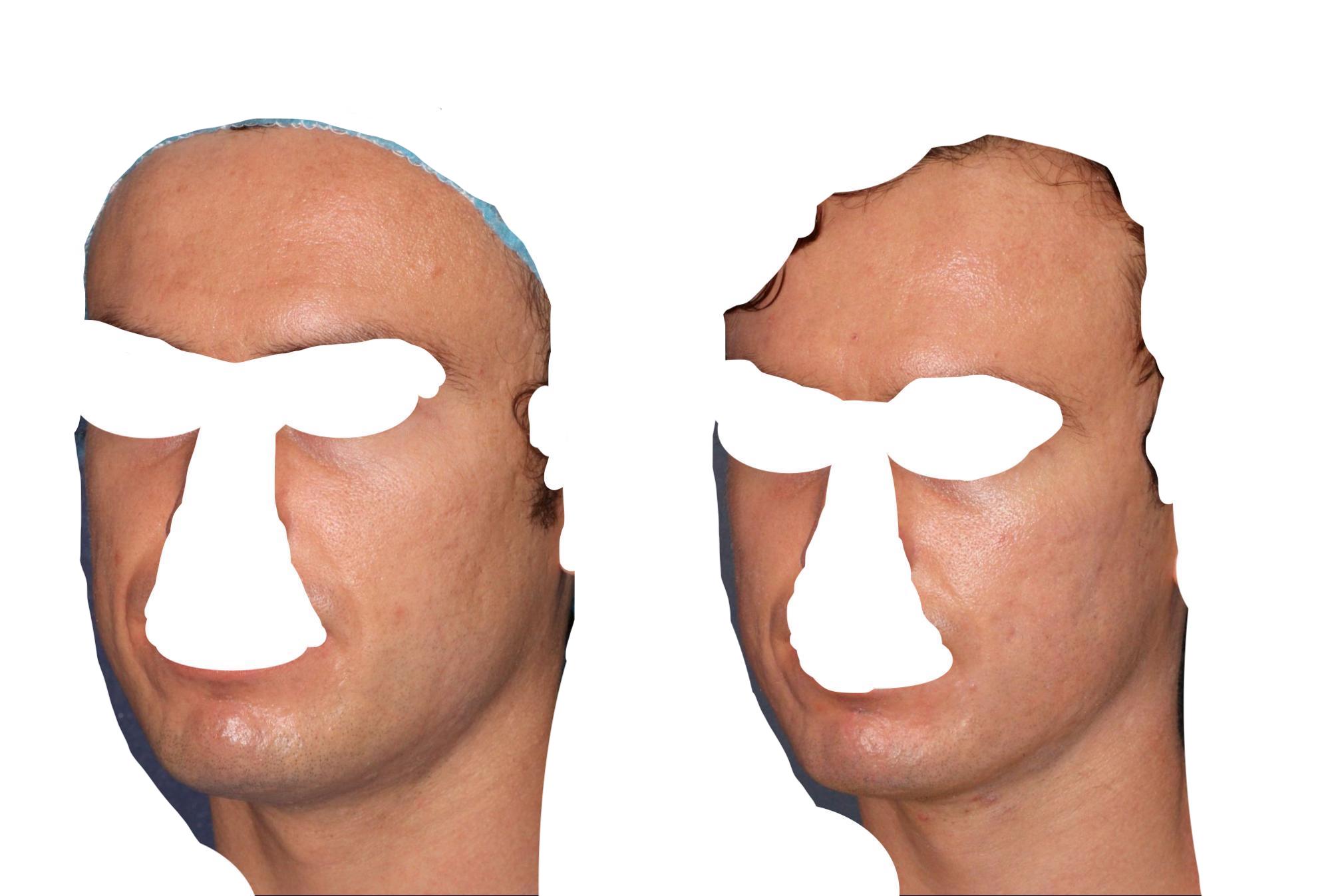
A significant feature of skin quality would be a lack of atrophic scars (what I came to Dr. Wu to treat), but the photos Dr. Wu took show that my pre-existing atrophic scars increased in depression and that new atrophies presented, which I highlight below in a grayscale version of Dr. Wu’s clinical photos zoomed in on the left cheeks:
|
|
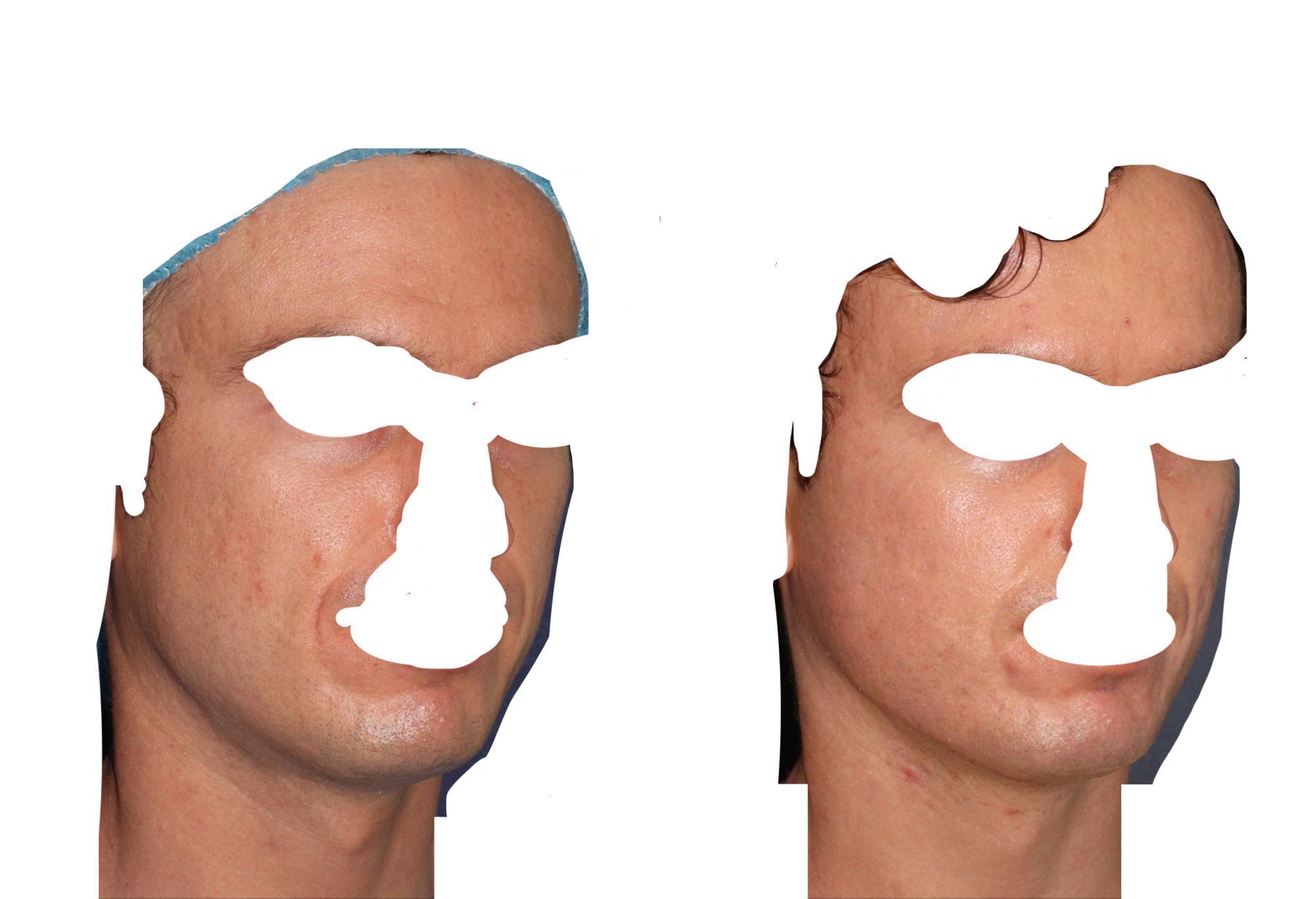
Another feature of skin quality is smoothness, which I show a clear deterioration in using the Canny edge detection algorithm, one of the most strictly defined methods for reliably detecting edges (i.e., delineations in smoothness in the gradient of an image) in computer science. It is widely applied in computer vision and is the basis for what is used in industry facial skin defect systems. Using the Canny implementation in the OpenCV package in the Python programming language↗ with parameters threshold1 and threshold2 being 75 and 150, respectively, I demonstrate below a clear increase in the number, size, and variability of edges detected in the “before” and “after” photos of the left cheek Dr. Wu used to assess progress, representing a decline in the smoothness of the skin:
A. Grayscale of Figure 19.A (Feb 8, ’21, before) cropped to left cheek | B. Canny-detected edges on Figure 24.A. Number of edge pixels = 2671 |
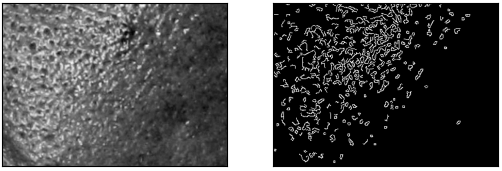
A. Grayscale of Figure 19.B (Jun 1, ’21, after) cropped to left cheek | B. Canny-detected edges on Figure 25.A. Number of edge pixels = 6866 |
To show this wasn’t just a fluke, I repeat the analysis on another pair of before and after photos from Dr. Wu’s clinic. This time I use the threshold parameters 150 and 300, respectively. The “after” photo was just 2 months after, and the damage only got worse.
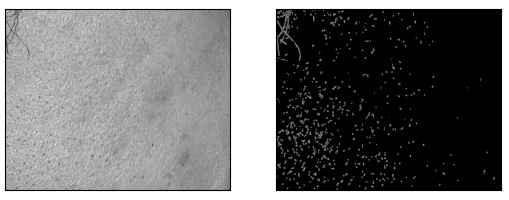
| A. Grayscale of before photo from Dr. Wu’s clinic on Feb 8, ’21 | B. Canny-detected edges on Figure 42.A. Number of edge pixels = 8591 |

A. Grayscale of after photo from Dr. Wu’s clinic on Apr 12, ’21. You can see the the increased depth of depressions between Figure 42.A. and this one too. | B. Canny-detected edges on Figure 43.A. Number of edge pixels = 18171 |
These degradations could be seen in many other parts of Dr. Wu’s photos and should be apparent to a trained eye. Furthermore, my continual attestations of these issues for months after (along with my own photos showing these issues) should have also warranted action by Dr. Wu to recognize and limit the scarring as early as possible. As these photos Dr. Wu used (Figures 19.B & 20.B) were only 4 months post, the issues continued to worsen since “Hypertrophic scarring usually occurs within 4 to 8 weeks following wound infection, wound closure with excess tension or other traumatic skin injury, has a rapid growth phase for up to 6 months, and then gradually regresses over a period of a few years, eventually leading to flat scars with no further symptoms” (Gauglitz et al., 2011). Weinstein et al. discuss hypertrophic scarring with direct relation to CO2 laser in writing “Hypertrophie [sic] scarring did not become evident until after 8 weeks. Scarring developed in two patients because of poor laser technique with too much overlap of pulses. Of the 13 patients with moderate scarring, secondary bacterial infection with S. aureus developed in three patients” (Weinstein et al., 1997).
🔗4.8. Further Concerns
I saw Dr. Wu in person Aug 4, 2021 because the texture had only worsened, despite his assurance it would improve on its own. He now did not know what to do to improve the results and he told me my skin looked great. I had red raised patches and didn’t get a chance to ask him about them, so the nurse said she would ask him to follow up with me, as she told me she also saw them in the photos. I didn’t receive any follow-up about my question, so I emailed him the next day:
Thanks very much for hearing my concerns yesterday. Your assistant mentioned she would ask you about one of the concerns I forgot to ask you about. There is a red raised patch on my left cheek she said she could see in the photos too. Does it look like some condition? I am wondering if everything I’m experiencing could be due to some allergic reaction? The only new topical I used after the procedure was the Skinmedica TNS recovery complex you recommended and I know it has fragrance. Is it a possibility? Also I didn’t see the most recent photos but it seems like my texture concerns developed after the before/after you sent me last email, which might coincide with when I switched from the Alastin to the TNS. I did ask you about some weird texture before but that was different. There wasn’t anything hypertrophic, to my memory.
I followed up in another email:
I note the allergy possibility because I have a history of topically induced allergy. There was a two-in-one sunscreen-lotion (lotion as in moisturizer) I tried once that covered my whole face in hives. I don’t recall what the name was but if this bumpy complexion is consistent with an allergic response and the redness that usually accompanies has mostly been masked by the post-laser redness, it all seems plausible to me. Then my question is: would having such a response for a while during the healing phase cause permanent damage?
Once again, Dr. Wu did not respond to either of my emails.
I emailed Dr. Wu again Aug 23, 2021 giving more info and photos about my condition after the CO2 laser, but he did not respond this time either.
I emailed Dr. Wu Mar 1, 2022, over a year post, to tell him I thought the pimples I formed after the procedure were actually a staph infection, which caused my complications. I included photos:
 |  |  |
A. Feb 22, ’21, 14 days post, clusters of papules below the lip, unresolved scabbing throughout beard | B. March 11, ’21, 1 month post, cysts and erythematous patches in beard | C. Apr 23, ’21, 2.5 months post, erythematous papules and lesions in beard and on chin, pronounced redness and irritation in the beard area with loss of hair follicles beginning to present |
He responded saying:
by the images you’ve shown me below, there is no evidence of such [staph]. Acne-like outbreaks following any sort of laser procedure are not uncommon and that’s exactly what is shown in your images. Staph infection of the skin presents as severe redness, pain, swelling and significant pus and exudate that typically forms a thick golden crust in areas that are infected. Patients are typically ill with fever and chills and the infection does not typically just go away without specific treatment. This isn’t something that typically just flies under the radar so to speak.
However, as I’ve previously shown, it is common knowledge in Dr. Wu’s field that infection after laser can easily “fly under the radar” and be confused with the expected sequelae of a laser, especially to less-experienced practitioners (Ramsdell, 2012b). Culton et al. write that nothing more than “papules and pustules after fractionated CO2 resurfacing should raise the suspicion of nontuberculous mycobacterial infection” (Culton et al., 2013). Furthermore, since I was never educated on the possbility of infection and how to identify it, I had no idea what to look for. I do not think it was appropriate for Dr. Wu to diagnose over email at any point after the CO2 laser without being certain his medical advice was accurate, especially when my concerns were easily attributable to serious complications. There were more occasions he did this on than the ones I have already mentioned in Sections 4.1, 4.2, 4.3, and 4.4, like on Feb 17, 2021, 9 days post, when I emailed him concerned about a large bump that had formed under my skin. He authoritatively informed me over email it was “just acute skin changes due to subcision/laser and is healing” and said to monitor it and that it would go down without offering to see me or asking any questions about it.
At the end of our relationship, Dr. Wu now said on March 3, 2022 “It’s possible that you are colonized by MRSA. A significant percentage of people are and remain completely asymptomatic. It may be useful to find out your colonization status at this time just for your own information and future reference”. This was the first time I learned about this and led me to wonder if it is so prevelant and could lead to outcomes like this, why did Dr. Wu not test me before the laser? I went ahead and got one of my pustules cultured and sensitivity-tested by dermatologist Dr. B.C. who confirmed normalcy.
The final time I saw Dr. Wu in person, Oct 18, 2021, I, visibly distressed, requested a mental health referral because of how much this had affected me. He simply said he didn’t know anyone who could help and left me on my own. Other reconstructive physicians argue mental health is an important aspect of scar treatments and that doctors providing them need to have a mental health specialist they can refer patients to.
🔗5. Getting Other Opinions
Realizing Dr. Wu was not there for me as much as I expected (either he did not understand what I meant or did not know what to do), I finally sought out other opinions almost 6 months after the CO2 laser on the face since Dr. Wu had kept telling me to wait the full 6 months. I had trusted his ability to diagnose and his professional opinion that this was all expected and would get better, until his timeline mostly passed and he made a new timeline encouraging me to wait a full year. I finally stopped ignoring my instincts due to my blind trust in Dr. Wu and sought other help.
🔗5.1. Dr. P.R.
I met Dr. P.R. in person Aug 2, 2021, and he told me the laser settings Dr. Wu had used were too strong (he requested my medical records from Dr. Wu’s office to confirm) and that the only thing to do now was wait, with more pulsed dye laser sessions to start to reduce the blood vessels feeding the inflammation. He diagnosed this primarily as post-CO2–laser fibrosis, which he differentiated from full-thickness scarring, along with some areas of full-thickness hypertrophic scarring resulting from the laser. He said once the laser vaporized all the water (the primary chromophore CO2 laser targets) in my skin, it burned the skin. He said he was experienced in diagnosing this, as he had seen it many times before.
🔗5.2. Dr. R.G.
On Aug 10, 2021, I saw Dr. R.G. who saw exactly the laser damage I had tried describing to Dr. Wu for months and prescribed a potent topical corticosteroid called Fluocinolone Acetonide .025% ointment twice a day for two weeks. When I went back, he thought there was improvement, but it was nowhere near resolved, and he told me there was nothing more he could do since a topical corticosteroid wasn’t administered soon enough.
🔗5.3. Realself
I also posted on a forum where doctors answer questions on September 7, 2021↗. My post read:
I got a fully ablative CO2 laser 7 months ago and have been struggling with a horrendous texture that appeared after and has seemingly worsened in the past 3 months. The skin is glossy/shiny. It has a rough texture with hypertrophic bumps everywhere. The skin doesn’t look like skin. I can only go outside at night. Is it post-laser milia? Is it scarring? Is it recoverable from?
I included the following before-after photos:
 |  |
Before (May 23, ’20) and after (Aug 31, ’21) photos I attached in my Realself question.
Plastic surgeon Dr. Connie Hiers responded: “You appear to have scarring from a laser treatment that was too deep for the area. PRP injections might be helpful to help rebuild some collegen [sic] or XoFlo injections once released.”
Dermatologic surgeon Dr. Amy Y. Paul also responded:
Thanks for your questions and photos. I am so sorry you are experiencing this skin change. This could be an unfortunate outcome because the laser was used in fully ablative mode. CO2 laser is much more safe and effective in fractionated mode, which lessens the risk of scarring significantly. I would recommend returning to your treating physician and see if there are other procedures that could help improve the skin texture. The original provider should be made aware of your skin changes so they can offer you some other options, possibly microneedling or some chemical peels, depending on your skin type. Please see an expert and best of luck!
🔗5.4. Dr. J.P.
Dr. J.P. seemed surprised about Dr. Wu performing fully ablative CO2 when he originally wrote back to me, “wow crazy story i have not touched a full field CO2 laser in 20 years. did a ton in the 90’s. i do a lot of deep full field sciton erbium work currently as well as fractional and some investigational work”. I saw Dr. J.P. January 7, 2022 and he diagnosed areas of scarring from the laser. He said the lasers and settings Dr. Wu used were extremely strong.
🔗5.5. Dr. A.B.
Dr. A.B. is senior to Dr. Wu at their practice, and I thought I would see him to help clarify matters. I saw him March 8, 2022. He claimed deep expertise regarding this treatment, informing me he helped develop the UltraPulse device. He told me it is clear I got an infection that went uncaught and that the scarring is permanent. He said it wasn’t nearly the worst he has seen, but he also said I will never again have normal skin like his assistant who was in the room. He said the delayed healing in the beard area that I had demonstrated to Dr. Wu 16 and 18 days post was a clear sign of infection. I asked how infection was possible with the prophylaxis and he said it didn’t cover all microbes. He asked if I had any pets and I informed him I did have an outdoor cat, and he said that was the most likely source, which I was never informed on the risks of with respect to this procedure. Pets are so common I don’t understand why I wasn’t provided more thorough prophylaxis. He recommended I go back to Dr. Wu for RF microneedling treatments to try to improve it. After the lack of care I had been treated with, I was pleasantly surprised by the candor Dr. A.B. exhibited rather than covering for his business partner.
🔗5.6. Dr. L.C.
I saw Dr. L.C. March 14, 2022 and she diagnosed my skin condition as “laser scarring” and said there was little that could be done now. She recommended I wait another year through the lifecycle of hypertrophic scarring as it would likely flatten to a degree on its own going forward.
🔗5.7. Dr. E.V. and Dr. H.B.
I saw rheumatologists Dr. E.V. and Dr. H.B. at UCLA March 16, 2022 to make sure I don’t have an underlying immune disorder like scleroderma that could have contributed to the outcome of the CO2 laser. They checked my immunoglobulins (IgG, IgM, and IgA) due to history of skin infection and confirmed normalcy. Scleroderma antibody panel was all negative. C-reactive protein was normal, meaning lack of inflammation in the body. Sedimentation rate, another marker of systemic inflammation, was normal. Other blood tests were normal (in relation to my blood disorder) too. They identified burn scarring and recommended massaging the area and consulting with their clinic’s dermatology department. 6.
🔗6. The Aftermath
I was ultimately left with hypertrophic scarring, loss of skin appendages (e.g., beard follicles), fat loss, long-lasting pruritus, loss of skin elasticity, hypopigmentation, and—seemingly contradictorily—hyperpigmentation. Some of these issues directly and indirectly leave my health compromised. Hypopigmentation, caused by a loss of melanin, leaves me with a higher likelihood of developing skin cancer (Brenner & Hearing, 2008). The treatments I must undergo to try to improve some of this damage leave me at risk of worsening these issues and developing new health issues. I demonstrate the issues the treatment left me with below.

A. May 18, ’20, 8.5 months before CO2 laser B. Feb 14, ’22, 1 year after CO2 laser. Extensive hypertrophic scarring, volume loss

A. Before CO2 laser B. Jun 22, ’21, 4.5 months post CO2 laser. Volume loss, hypertrophic scarring

A. 4 days post CO2 laser B. Mar 13, ’22, 13 months post CO 2 laser. Persistent hyperpigmentation extending the exact boundary of the treated area

Aug 23, ’21, 6.5 months post laser. Loss of hair follicles as well as scarring stopping at edge of treated area

Jul 14, ’21, over 5 months post CO2 laser. Hypopigmentation stopping at edge of treated area

Jun 30, ’22, over 16 months post laser. Loss of hair follicles as well as scarred texture stopping at the edge of the treated area

Sep 16, ’21, over 7 months post CO2 laser. Scarred texture with normal texture in untreated areas (mustache, immediately below lip, and part of chin)

Feb 13, ’22, 1 year post. Extensive hypertrophic “orange peel” texture
 |  |  |
The two circled areas show areas Dr. Wu did not apply the laser, which have normal texture and tone after (Jul 26, ’21 and Aug 17, ’21). Scarring clearly stops at the bottom edge of the treated area on the jaw.
 | 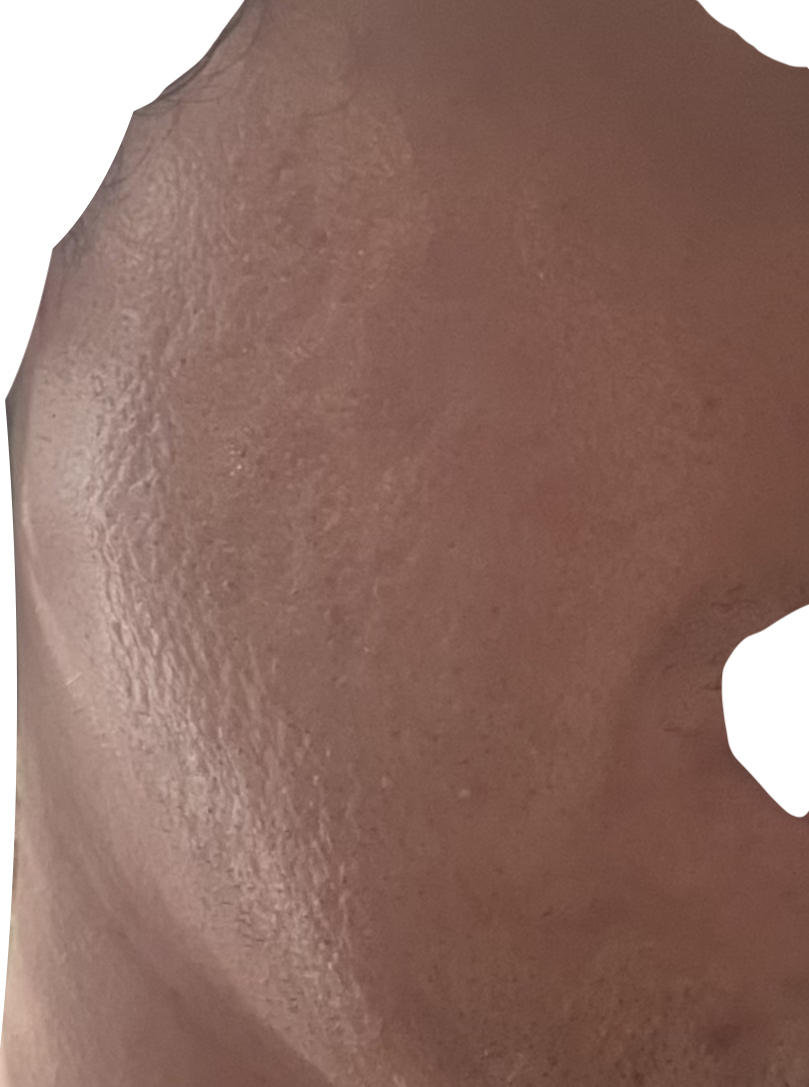 |
A. Before photo taken Aug 4, ’20, 6 months pre-laser. B. After photo taken and sent to Dr. Wu Jan 30, ’22, 1 year post, highlighting new hypertrophic texture throughout the lower cheek, ending at the treatment boundary.

Jan 31, ’22, 1 year post. Line showing demarcation between treated area above (hypertrophic bumps) and untreated below

Aug 31, ’21, 7 months post. Feathering in sideburn area shows transition between scarred/treated area and untreated area. A more stark delineation can be seen below the jawline.

May 14, ’20, 9 months before and Feb 13, ’22, 1 year post.
 |  |
Feb 12, ’21, 4 days post and Apr 13, ’22, over 1 year post. The circled area where aggressive settings were applied in the jawline shows the most notable scarring.
Dr. Wu only seemed receptive to recognizing complications after I cited what multiple other doctors told me, whereas he had initially dissuaded me from getting other opinions in telling me “too many opinions can sometimes muddy the waters” and insinuated other doctors were wrong. After I had finally convinced him of the complications resulting from this procedure, he wrote to me “I think a biopsy would be a good idea” on Feb 14, 2022. Every other doctor I saw explicitly advised against a biopsy when I brought it up, explaining that the findings would not change the treatment strategy and would just leave another scar. This seems to speak to Dr. Wu’s unique judgment and guidance. Dr. Wu never once informed me of the option of a topical corticosteroid to limit the inflammation and thereby the scarring, which is an essential first line of treatment when scarring begins to present after this procedure↗ (Metelitsa & Alster, 2010), which I feel I demonstrated the symptoms of to him time after time without knowing it was scarring myself. After I told him Dr. R.G. had prescribed me the potent topical corticosteroid, Dr. Wu finally prescribed a calcineurin inhibitor to try to further ameliorate damage, but it seemed largely too late since that was 8 months after the laser.
Dr. Wu never reached out to me to try to figure out what went wrong as part of any post-accident root-cause analysis to limit the chances of this happening again. I hope that publishing my story can prevent future patients’ outcomes being left to chance.
I was 25 when Dr. Wu performed this laser on me. I was a fully functional young adult who had just a year and a half prior graduated with honors from university on a full scholarship. I had friends and partners. I was no doctor, but I tried to do good with my skills. I volunteered regularly, teaching underprivileged kids science, engineering, and more. I had a job where I cowrote a tool enabling millions of others to manage their businesses, nonprofits, education, and more. I was optimistic and had no history of mental issues, use of antidepressants, or substance abuse.
And now I have completely isolated myself. I haven’t had the courage to go outside for over two years. I had to take extended medical leave from work and am at risk of losing my job (and more) altogether, as I’m rarely able to focus due to the trauma. I have had to pass up other career and life opportunities. I have sought out psychological help—without the assistance I requested from and was denied by Dr. Wu—and been diagnosed with major depressive disorder, PTSD, agoraphobia, and body dysmorphia. Before entering a stage of acceptance, I couldn’t sleep and would wake up from night terrors. This abrupt deterioration in my appearance and the bleak search for answers overwhelmed me to the point of ideating suicide for the first time in my life, occupying my mind every single day for many months.
🔗7. Trouble Getting Medical Records
When I first began to suspect Dr. Wu had likely done a fully ablative CO2 laser on my face, I emailed him April 21, 2021 (2.5 months post) requesting procedure info, asking “Would you mind giving me some info on the face laser(s) you did?” Dr. Wu did not respond to me.
Months later, I tried again, calling Dr. Wu’s office to get my medical records to give other doctors to help them assess my condition. His office made it relatively expensive to receive them directly, telling me it would cost $20 for the written records and $5 per photo (photos being the only diagnostic I think Dr. Wu employed in my case). They, however, informed me they would send them directly to another doctor’s office for free. I therefore had Dr. P.R. request them, but Dr. Wu (who prepared the records) did not send him the record of the CO2 laser on my face, which was clearly the one Dr. P.R. and I were most interested in. I emailed Dr. Wu directly to address this, and he finally sent it to me, claiming oversight. There were many other records, like my consent forms, that Dr. Wu did not send either. In addition, Dr. Wu did not send Dr. P.R. any of my photos.
Dr. Wu’s office made me directly request my photos, even though his office staff confirmed they are part of my medical record which is what Dr. P.R. requested on my behalf, and charged me $150 for what they said would be 113 photos—they ended up sending me 96 unique photos. This pricing does not seem consistent with the 25 cents per page plus a reasonable clerical cost (I believe this clerical cost came out to $126 of the $150) that California law allows for medical records↗. The process was so difficult that I did not pursue getting the remaining records they omitted.
🔗8. “Double Board Certification”
Dr. Wu’s bio reads “Douglas C. Wu, MD, PhD is a double board-certified dermatologist in both Canada and the USA”↗. Dr. Thomas Nakatsui, a dermatologist with current board certifications in Canada and the US, says “Being certified in both Canada and the USA is not precisely the same as being double board certified. Usually when doctors speak of being double board certified, it means they have embarked on training in two different areas of medicine that are governed by different boards”. He gives the example of a colleague who “has received certification in both Pathology and Dermatology and thus is double board certified. If he was certified in both of these areas in both Canada and the USA, he would not claim he was quadruple board certified”↗.
Furthermore, as of October 23, 2023, Dr. Wu claims he is a “proud member” of the Royal College of Physicians and Surgeons of Canada on his profile for his practice in Canada↗ and lists that he is a fellow of the Royal College of Physicians and Surgeons of Canada again on his profile for his practice in the US↗. However, he is not listed in their directory↗. I therefore emailed them to verify, and they wrote back the same day, “Dr. Wu is not listed on the Royal College Directory as he is not a Fellow (member) of the Royal College currently.” They followed up explaining, “Being a Fellow/member is voluntary. As a Fellow Dr. Wu would have the FRCPC designation, enrollment in the MOC Program and pay annual dues.” The MOC (Maintenance of Certification) Program requires routinely completing continuing education activities↗. By indicating he is a member, patients are misled to believe that he is keeping up with those reponsibilities and is therefore a more knowledgeable doctor.
🔗9. A Call for Restrictions on Who Can Perform Ablative CO2 Laser
Whether fractionally or fully ablative, I now know CO2 laser is an invasive surgery (not just an in-office procedure, even though many clinics downplay it as such) with significant risks. I was not aware it is surgery, for my back or face. The issue of misclassification, misinformation, and/or withholding information is prevelant for this surgery and some doctors claim it is nonsurgical. However, the American Medical Association defines surgery as “the diagnostic or therapeutic treatment of conditions or disease processes by any instruments causing localized alteration or transposition of live human tissue which include lasers, ultrasound, ionizing radiation, scalpels, probes, and needles”. It goes on to qualify laser or light-knife surgery as invasive↗. Others express feeling deceived by other clinicians, like someone who writes “never once told me its [sic] considered a surgery” under a review on Realself titled “Laser Resurfacing (CO2 Laser) Ruined my Life”↗.
The potential upside of this surgery does not seem particularly significant, especially in cases like mine (other skin surgeons advised they would have never recommended such a treatment for me and many choose not to perform CO2 laser at all), but the potential downside is life-alteringly devastational. The consequences can cost one’s life, either directly through an infection, for example, or indirectly through the psychological aspects of iatrogenic scarring that so obviously concerns someone who wants to reconstruct one’s skin in the first place. On this journey, I’ve encountered others who have experienced similar complications from the same surgery and suffered similar debilitation. One of them is around my age and was ironically starting medical school; however, they withdrew indefinitely. Another is also the same age and in school. They switched to permanent online education because of the impacts this has had on them.
I therefore urge for additional oversight for CO2 laser surgery. A model similar to the iPledge REMS safety program, in which doctors must become federally authorized to prescribe isotretinoin and those who have been negligent lose that privilege, seems like it could provide patients much-needed safety standards for a procedure I have found to have such a high rate of complication. Manuskiatti et al. documented a 3.8% incidence of scarring for CO2 laser in the 1990s (Manuskiatti et al., 1999). Today, UltraPulse Active FX carries a 61% satisfaction rate↗, among the lowest across all cosmetic procedures, on Realself, a cosmetic-procedure review site.
This information was originally available at https://www.realself.com/reviews/ultrapulse-CO2-laser/nonsurgical/active-fx↗ but that URL has changed to https://www.realself.com/nonsurgical/ultrapulse-co2-laser#activefx↗ and they explicitly hide the satsifaction score for ActiveFX there now (whereas they show the satisfaction score for DeepFX). Also note that Realself calls this procedure nonsurgical, as can be seen in the URL.
In a study of CO2 laser to improve burn scars, Ozog et al. had 8 of 18 (44%) patients drop out after the first of three treatments due to complications like pain, infection, and ulceration (Ozog DM, 2013). In another study treating eyelids of nine patients with ablative fractional laser (CO2 and Erbium:YAG), 41% of patients ended up with permanent scars, requiring blepharoplasty to try to correct (Fitzpatrick et al., 2000). Wind et al. found that dermal fibrosis resulted in 4 out of 8 ablative fractional laser patients, questioning if it is to “be regarded as dermal remodeling or a subtle subclinical form of scarring” (Wind et al., 2012), which I believe gives just a glimpse at the potential upper range of the true rate of complication for this kind of surgery.
I also hope for regulations that better protect a patient’s right to informed consent. No patient should be given consent forms under the influence of incapacitating intoxicants immediately pre-procedure. A patient should not be rushed by the healthcare provider to just sign those forms without reading them. The doctor should go over them with the patient and gauge that the patient’s understanding is adequate. Upon signing, the patient should be given a copy to refer back to. Furthermore, the patient or authorized requestor should be given this copy when requesting complete medical records. I don’t think any of these things were done like I think they should have been in my case.
🔗10. Conclusion
In conclusion, I feel that I followed all of the minimal advice Dr. Wu gave me and was communicative throughout about anything I was not informed on and had questions about. I repeatedly brought up concerns pre-, intra-, and post-op that I feel were brushed off or flat out ignored. When I later asked him if he had ever seen this complication, Dr. Wu said no. When I asked if he had ever even heard of it, he said of course it is something taught in school but that is exceedingly rare. Dr. Wu’s assurance that everything was normal (oftentimes over email and without adequate diagnostics) and advice to wait 6 months for my concerns to resolve kept me from seeking out another opinion until it was too late. On September 16, 2021, I emailed Dr. Wu asking “Have you consulted with any of your colleagues about my case? I can pay for any related costs, if you think it could help. I should have asked a long time ago but I didn’t want to undermine your authority in any way.” Dr. Wu responded with a very generic answer that made me doubtful he did: “I consult with my colleagues frequently about all manner of cases. Pride is never an issue and I’m absolutely not concerned about any monetary compensation from your end, although I appreciate your consideration in asking and offering. Your health and well-being is my only priority.” I had offered to pay for his time responding to my emails before as well because of how often he didn’t (oftentimes having CC’d his assistant too), but he refused, ending our relationship with a ~63% email response rate. When I finally began to consult with other doctors and educate myself on this procedure having no medical background, it became clear even to me that the standard of care commensurate with the intensity of this procedure, like simply adhering to instructions in the device’s operator manual, significantly differed from my experience. Dr. Wu touts an impressive resume↗, but I’ve learned that says nothing about his skill as a clinician. He was not the right clinician to take care of me for such a common concern, leaving me with extensive burn scarring throughout my face, along with lifelong trauma. Please be careful about who you let take care of you.
🔗11. Reporting the Incident
🔗FDA
I submitted an adverse event report to the FDA↗, which compelled the manufacturer to investigate the incident. In their response↗ they concluded there was no device malfunction but their medical director validated what happened to me as “a serious injury due to a large area of hypertrophic scars on the face”.
🔗Medical Board of California
I also submitted a complaint about Dr. Wu, which contained much of the info on this site, to the Medical Board of California. It was apparently investigated, but after nearly a year they closed the case without taking any action or following up with me for any additional info or testimony.
 |  |  |
Step 1
 |  |  |
Step 2
 |  |
Step 3
🔗Online Reviews
Lastly, I attempted leaving online reviews, but review platforms often reject or hide negative reviews because the businesses are their customers.
🔗Healthgrades
My review was rejected for containing inappropriate content. Their community guidelines↗ mention any review that is “inflammatory”, which is a completely subjective term, is in violation.
🔗Realself
My review there↗ was published promptly.
Google hid my review for Dr. Wu↗ and Cosmetic Laser Dermatology↗ until I removed the photos.
🔗BBB
BBB published a redacted version of my review on Dr. Wu’s company’s profile↗. It doesn’t seem to affect the company’s A+ rating.